1. Introduction to Upper Limb Rehabilitation after Stroke
Upper limb impairment is a common and often challenging consequence for many individuals following a stroke within the UK. These difficulties can range from subtle weakness and decreased coordination, to profound loss of movement and sensation in the shoulder, arm, or hand. For people living in the UK, where independent daily living and quality of life are highly valued, such impairments can significantly affect the ability to manage everyday activities—from making a cup of tea to dressing oneself or using public transport. In the context of the NHS, upper limb rehabilitation forms an essential part of post-stroke care, aiming not only to restore function but also to support dignity and autonomy for survivors. By understanding the scale and impact of upper limb impairment after stroke, both clinicians and families can appreciate the vital role that personalised exercise prescription plays in the journey toward recovery and participation in meaningful life within UK society.
2. The Role of the NHS in Post-Stroke Rehabilitation
The National Health Service (NHS) plays a pivotal role in supporting stroke survivors throughout their rehabilitation journey, particularly when it comes to upper limb recovery. The NHS provides a comprehensive network of services designed to address the complex and evolving needs of individuals who have experienced a stroke. This holistic approach is facilitated by multidisciplinary teams (MDTs) and well-structured care pathways that ensure each patient receives tailored support from hospital admission to community reintegration.
Examination of NHS Services for Stroke Survivors
Following an acute stroke, patients are typically admitted to specialist stroke units within NHS hospitals. These units offer immediate medical management, early assessment, and timely initiation of rehabilitation. As patients stabilise, rehabilitation becomes increasingly central to care, focusing on regaining function and promoting independence. NHS services commonly provided include:
| Service | Description |
|---|---|
| Acute Stroke Units | Specialist medical and nursing care with early access to physiotherapy and occupational therapy. |
| Inpatient Rehabilitation Wards | Intensive therapy programmes tailored to individual recovery goals. |
| Early Supported Discharge (ESD) | Enables suitable patients to continue rehabilitation at home with ongoing input from a community MDT. |
| Community Rehabilitation Services | Outpatient or home-based therapy supporting longer-term functional improvement. |
| Follow-Up Clinics | Regular reviews by consultants, therapists, and specialist nurses to monitor progress and adjust treatment plans. |
The Multidisciplinary Team Approach
Effective upper limb rehabilitation within the NHS relies heavily on collaboration among healthcare professionals. The core members of the MDT often include:
- Physiotherapists: Specialise in movement and physical recovery, including upper limb exercises.
- Occupational Therapists: Focus on practical skills for daily living and fine motor function.
- Speech and Language Therapists: Support communication and swallowing difficulties, which can indirectly affect overall rehabilitation engagement.
- Nurses: Provide ongoing care and monitor health needs.
- Consultants (Stroke Physicians/Neurologists): Oversee medical management and coordinate long-term planning.
- Psychologists: Address emotional wellbeing, which is crucial for motivation during exercise prescription.
Typical Care Pathways for Upper Limb Rehabilitation after Stroke
The NHS strives for continuity of care through defined pathways that transition patients smoothly across different settings. A typical pathway may look like this:
| Stage | Description of Care Provided |
|---|---|
| Hospital Admission & Acute Phase | Immediate assessment; initiation of early mobilisation and gentle upper limb exercises as appropriate. |
| Inpatient Rehabilitation | Daily intensive physiotherapy and occupational therapy targeting upper limb function. |
| Discharge Planning & Early Supported Discharge (ESD) | Assessment for home-based rehabilitation; development of personalised exercise prescription by the MDT. |
| Community-Based Rehabilitation | Sustained therapy interventions; periodic review by therapists; adaptation of exercises based on progress. |
| Long-Term Follow-Up & Self-Management Support | Ongoing advice, encouragement, and resources for continued upper limb exercise at home or in local groups. |
A Compassionate Continuum of Care
This coordinated approach ensures that every stroke survivor under the NHS has access to consistent, evidence-based care—tailored not only to their physical needs but also to their emotional wellbeing. By fostering teamwork across disciplines and settings, the NHS empowers individuals to achieve their best possible recovery in a supportive environment familiar with UK values of equity and community care.
3. Principles of Exercise Prescription for Upper Limb Recovery
In the context of upper limb rehabilitation following a stroke within the UK NHS, developing an effective exercise prescription is anchored in a set of core principles. These principles are shaped not only by clinical evidence but also by national guidelines such as those provided by the National Institute for Health and Care Excellence (NICE) and the Chartered Society of Physiotherapy (CSP). The approach is always person-centred, respecting each individuals unique journey to recovery.
Core Principles of Exercise Prescription
A tailored exercise programme begins with a thorough assessment of the individuals current ability, functional limitations, and personal goals. Safety comes first: it is essential to consider the presence of co-morbidities, risk of falls, fatigue levels, and cognitive capacity before introducing or progressing exercises. Exercises are selected to facilitate active participation, encourage neuroplasticity, and promote independence in daily activities.
UK-Specific Guidelines
Within the NHS, clinicians draw upon evidence-based recommendations such as those outlined by NICE. These advocate for early intervention where appropriate, regular reassessment, and an interdisciplinary approach involving physiotherapists, occupational therapists, and other allied health professionals. Programmes typically blend task-specific practice—such as reaching or grasping—with strength training, stretching, and functional tasks relevant to UK lifestyles.
Safety, Individual Goals, and Progression
Safety remains paramount throughout all stages of rehabilitation. Professionals continually monitor for signs of pain or fatigue and modify exercises as needed. Goal-setting is collaborative; individuals are encouraged to identify meaningful objectives—whether that’s making a cup of tea independently or returning to gardening. As recovery progresses, exercises are adjusted in intensity and complexity to ensure ongoing challenge without compromising safety. This careful progression supports both physical improvement and psychological confidence on the path towards greater independence.
4. Types of Exercises Recommended in NHS Practice
Following a stroke, upper limb rehabilitation within the UK NHS is rooted in evidence-based, patient-centred approaches that prioritise both safety and functional recovery. A wide variety of exercises are prescribed by physiotherapists and occupational therapists, tailored to individual needs and abilities. These often combine traditional techniques with newer, technology-assisted interventions to help maximise each person’s potential for regaining independence.
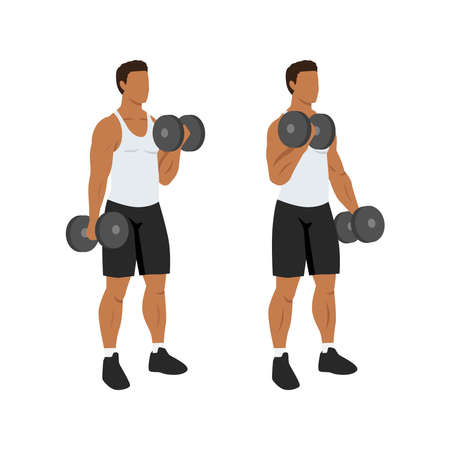
Commonly Prescribed Exercises
Therapy usually incorporates a blend of movement-focused and task-oriented exercises. These aim to address specific impairments such as weakness, reduced coordination, or spasticity, while also encouraging participation in meaningful activities. Below is an overview of some frequently recommended exercise types:
| Exercise Type | Description | Example Activities |
|---|---|---|
| Passive Range of Motion (PROM) | Assisted movements performed by a therapist or carer to maintain joint flexibility when active movement is limited. | Shoulder flexion and extension; wrist rotations |
| Active-Assisted Exercises | The patient initiates movement with support as needed from another person or equipment. | Supported arm lifts using a sling or table surface |
| Active Range of Motion (AROM) | Movements carried out independently to improve muscle activation and control. | Reaching tasks; opening and closing the hand |
| Strengthening Exercises | Progressive resistance activities to rebuild muscle strength and endurance. | Squeezing therapy putty; lifting light objects |
| Functional Task Practice | Simulated daily living tasks to promote real-world skill use. | Peg boards; dressing practice; pouring water into a cup |
| Sensory Re-education | Activities designed to retrain touch and proprioception. | Handling textured materials; object recognition games |
| Technology-Assisted Therapy | The use of devices or digital tools to enhance engagement and feedback. | Virtual reality games; robotic-assisted movement training; home exercise apps approved by the NHS |
NHS Therapy Approaches: A Holistic Perspective
NHS practice not only focuses on the repetition of movement but also integrates these exercises within daily routines. Therapists encourage patients to perform exercises regularly at home, sometimes providing written or digital exercise programmes. Where appropriate, group sessions are offered in community settings, fostering peer support and motivation—a valued aspect of British rehabilitation culture.
Combining Traditional and Modern Methods
The NHS continually adapts its recommendations in line with emerging research and available resources. While hands-on therapy remains essential, many services now offer technology-supported options for those able to access them. This blended approach helps ensure that rehabilitation is inclusive, accessible, and tailored to each individual’s journey towards recovery.
5. Integration of Rehabilitation into Everyday Life
Making Upper Limb Exercises Part of Daily Routines
Successful upper limb rehabilitation after stroke relies not only on structured sessions with NHS therapists, but also on consistent practice at home. Incorporating exercises into daily life can feel daunting, yet small adjustments often make a significant difference. Try linking specific movements to regular activities—for example, reaching for a cup during tea time or stretching your hand while dressing. Setting gentle reminders or using post-it notes in visible places can prompt you to practise targeted movements throughout the day.
Practical Tips for Home-Based Exercise
Choose familiar settings for practice, such as the kitchen table or living room. Use everyday objects: squeeze a soft ball while watching telly, or practise grasping and releasing coins from your purse. Consistency is key; short, frequent bursts—five to ten minutes at a time—are usually more effective than longer, infrequent sessions. Celebrate small achievements, as each bit of progress builds confidence and motivation.
Support from Family and Care Partners
Family members and care partners play a vital role in creating an encouraging environment. Gently prompt the person recovering from stroke to engage in their exercises, but avoid pressuring them. Participate together where possible; this might mean joining in with arm stretches or assisting with safe hand-over-hand guidance if needed. Remember, patience and reassurance foster both emotional wellbeing and physical improvement.
Building Exercise into Social Activities
In the UK, community groups and social clubs may offer gentle group activities suitable for stroke survivors—such as seated exercise classes or crafting sessions that use fine motor skills. Attending these together not only supports rehabilitation but also helps combat isolation. Ask your local NHS rehabilitation team for recommendations about suitable groups or accessible venues nearby.
Adapting Everyday Tasks for Rehabilitation
Think creatively about adapting household chores: folding laundry, stirring ingredients for baking, or gardening tasks like potting plants all provide natural opportunities to use and strengthen the affected arm. Breaking tasks into manageable steps can make them less overwhelming and more achievable.
Encouragement and Long-Term Habits
Lastly, remember that recovery after stroke is often gradual and requires ongoing effort. Gentle encouragement from loved ones, combined with practical integration of exercises into everyday life, makes the journey less isolating and more hopeful. By weaving upper limb rehabilitation into daily routines within the supportive framework of the UK NHS, individuals are empowered to regain independence and enjoy meaningful improvements in their quality of life.
6. Support Networks and Community Resources
Recovery from stroke, particularly when it comes to upper limb rehabilitation, is a journey best undertaken with strong support and access to reliable resources. Within the UK, the NHS is complemented by a wealth of community-based services, support groups, and online platforms designed specifically for stroke survivors and their families.
Overview of UK-Based Support Groups
Numerous organisations across the UK offer invaluable peer support and guidance. The Stroke Association is one of the largest, providing local groups where individuals can share experiences, attend exercise classes tailored to upper limb rehabilitation, and receive encouragement in a warm and understanding environment. Many local NHS trusts also collaborate with community centres or charities to facilitate group sessions aimed at building confidence and social connections post-stroke.
Online Resources for Ongoing Guidance
The digital landscape has greatly expanded the resources available to stroke survivors. Trusted websites such as the NHS Choices portal offer practical advice on prescribed exercises, video demonstrations, and tips for adapting activities of daily living. Additionally, apps like MyTherapy or tools provided by the Different Strokes charity empower individuals to track progress and maintain motivation between formal therapy sessions.
Local Services and Tailored Assistance
Across the UK, many councils and health authorities commission local services that complement NHS care. Occupational therapists often work closely with community teams to provide home visits, adapting exercise plans to suit each person’s living environment. Local leisure centres may offer gentle exercise classes suitable for those recovering strength and mobility in their arms, while transport schemes or volunteer drivers help reduce barriers to participation.
For families and carers, carer support groups (such as those run by Carers UK) are available to address emotional needs and provide practical information about navigating the healthcare system. It’s always worth asking your GP or hospital team about what’s available in your area—there is a network of people ready to walk alongside you through every stage of recovery. By tapping into these resources, both survivors and their loved ones can feel supported and empowered throughout the rehabilitation process.


