Introduction to Spinal Mobilisation and Manipulation
Spinal mobilisation and manipulation are key approaches within manual therapy, offering non-invasive methods for addressing musculoskeletal discomfort, especially back and neck pain. These hands-on techniques have evolved over time, gaining recognition as effective components of holistic healthcare. In the UK, both spinal mobilisation and manipulation have become increasingly integrated into mainstream clinical practice, reflecting a growing trust in their safety and efficacy. Mobilisation typically involves gentle, controlled movements of the spine to improve mobility and reduce stiffness, whereas manipulation refers to quicker, more forceful movements designed to restore joint function. The development of these therapies can be traced back through centuries of traditional healing practices, but it is only in recent decades that rigorous scientific study and professional regulation have established their place within the British healthcare landscape. Today, physiotherapists, osteopaths, and chiropractors across the UK utilise these methods as part of evidence-based treatment plans tailored to individual needs. Their acceptance has been strengthened by the support of national health bodies and professional organisations, ensuring high standards of care and patient safety. As we begin to explore spinal mobilisation and manipulation in greater depth, it’s important to understand how these therapies have come to be trusted allies in supporting mobility and wellbeing throughout the UK.
2. The Science Behind Manual Therapy
Spinal mobilisation and manipulation are grounded in a rich understanding of both anatomy and physiology, forming the cornerstone of manual therapy approaches commonly employed within British clinical settings. These interventions are designed to restore mobility, reduce pain, and improve function, drawing upon evidence-based principles that prioritise patient safety and well-being.
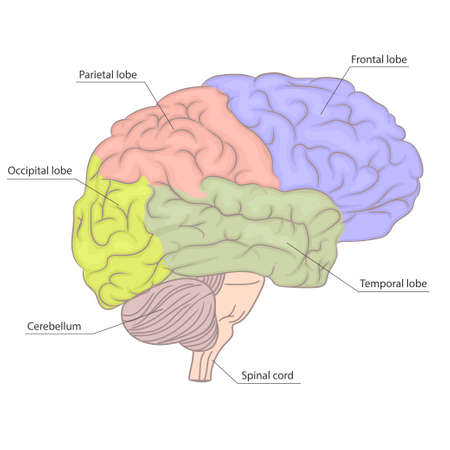
Anatomical Foundations
The human spine is a complex structure composed of vertebrae, intervertebral discs, ligaments, muscles, and nerves. Each component plays a pivotal role in maintaining stability and facilitating movement. In British practice, manual therapists pay particular attention to:
- Segmental mobility: Assessing each vertebral segment’s range of motion
- Soft tissue integrity: Evaluating muscle tone and ligamentous support
- Nerve pathways: Ensuring neurological structures remain uncompromised during interventions
Physiological Principles
Manual therapy aims to influence physiological processes such as pain modulation, inflammation reduction, and neuromuscular control. Techniques like spinal mobilisation involve gentle oscillatory movements that can promote fluid exchange and relax hypertonic muscles, while manipulation delivers a precise, controlled thrust intended to restore joint alignment and function.
Evidence-Based Outcomes in the UK
| Intervention | Primary Benefit | Supporting Evidence (UK Context) |
|---|---|---|
| Spinal Mobilisation | Pain reduction; improved flexibility | NICE guidelines recommend for persistent lower back pain; supported by NHS clinical audits |
| Spinal Manipulation | Restoration of joint mobility; neurological benefits | Cochrane reviews highlight short-term relief in musculoskeletal conditions; widely used by British physiotherapists and osteopaths |
Relevance to British Practice
The integration of spinal mobilisation and manipulation into British healthcare is informed by ongoing research, professional standards from bodies such as the Chartered Society of Physiotherapy (CSP) and General Osteopathic Council (GOsC), as well as patient-centred values. Practitioners strive to tailor interventions based on individual assessments, respecting the unique anatomical and physiological needs of each person while adhering to evidence-based guidelines for optimal outcomes.
3. Clinical Application and Indications
Spinal mobilisation and manipulation are gentle yet effective manual therapy techniques that play a significant role in the management of musculoskeletal conditions within the UK. The careful application of these interventions is guided by both clinical judgement and established best practice recommendations, ensuring patient safety and optimal outcomes.
Common Conditions Addressed in UK Practice
These techniques are most frequently utilised for patients presenting with non-specific low back pain, mechanical neck pain, and certain types of thoracic discomfort. In the UK, clinicians may also employ spinal mobilisation for individuals with age-related stiffness or degenerative joint changes, such as those seen in osteoarthritis. Manipulation, when indicated, can be considered for acute episodes of restricted movement or pain that have not responded to more conservative measures.
Indications for Spinal Mobilisation
Spinal mobilisation is often recommended where gentle, controlled movement is needed to improve joint function, reduce muscle guarding, and alleviate discomfort. It is particularly suitable for older adults or those who may be anxious about more forceful interventions. Best practice suggests beginning with lower grades of mobilisation, always considering patient feedback and individual tolerance.
Indications for Spinal Manipulation
Spinal manipulation may be appropriate for younger, otherwise healthy individuals experiencing sudden-onset restriction or locked joints, especially when there are no signs of serious underlying pathology. In line with UK guidelines, manipulation should only be performed after thorough assessment and screening for contraindications such as osteoporosis or neurological compromise.
Best Practice Recommendations
The National Institute for Health and Care Excellence (NICE) provides guidance on the use of manual therapies, emphasising shared decision-making and a patient-centred approach. Practitioners are encouraged to combine manual therapy with exercise and education for long-term benefit. Regular review and adaptation of treatment plans are essential to ensure ongoing appropriateness and effectiveness. Ultimately, careful communication and gentle encouragement help patients feel supported throughout their recovery journey.
4. Patient-Centred Considerations
In the context of spinal mobilisation and manipulation, a patient-centred approach lies at the heart of best practice within manual therapy. In the UK, healthcare professionals are guided by the principles of respecting individual needs, values, and preferences—cornerstones that shape effective and compassionate care.
Personalising Therapy for Each Individual
Every patient presents with a unique combination of symptoms, medical history, lifestyle factors, and expectations. As such, tailoring therapy is not only clinically beneficial but also aligns with British values of dignity and respect. Manual therapists are encouraged to conduct thorough assessments and engage in meaningful conversations with their patients to understand what matters most to them.
Key Areas to Personalise
| Consideration | Examples in Practice |
|---|---|
| Pain Tolerance | Adjusting technique intensity to suit comfort levels |
| Lifestyle Factors | Adapting recommendations for work, home, or leisure activities |
| Cultural Beliefs | Respecting views on touch or certain interventions |
| Communication Preferences | Offering verbal explanations, written information, or visual aids as needed |
Respecting Patient Preferences and Shared Decision-Making
Shared decision-making is a hallmark of UK healthcare. This means involving patients in choices about their care by providing balanced information and supporting autonomy. Patients are encouraged to express their concerns, goals, and any hesitations they may have regarding manual therapy techniques. Practitioners should foster an open dialogue where questions are welcomed and decisions are made collaboratively.
Incorporating British Values into Care
- Dignity: Ensuring all interactions uphold patient dignity regardless of age or background.
- Respect: Listening actively and valuing patient input during every session.
- Empowerment: Encouraging self-management strategies alongside hands-on interventions.
- Transparency: Explaining potential risks, benefits, and alternatives in clear, accessible language.
Navigating Sensitive Topics with Compassion
The gentle nature of British communication supports sensitive discussions around discomfort or anxiety related to spinal mobilisation or manipulation. Practitioners can reassure patients by acknowledging their feelings and offering options that honour their boundaries.
This thoughtful, patient-centred approach ensures that manual therapy remains a positive experience rooted in trust—fostering better outcomes and supporting holistic well-being throughout the journey of care.
5. Risks, Safety and Professional Standards
When considering spinal mobilisation and manipulation, it is essential to approach these manual therapy techniques with a balanced understanding of both their benefits and potential risks. While many individuals experience significant relief through these interventions, it is important to be aware that, as with any therapeutic procedure, there are inherent risks that must be carefully managed.
An Honest Look at Potential Risks
Manual therapy involving the spine can occasionally result in adverse effects such as mild soreness, stiffness, or discomfort following treatment. More serious complications—such as nerve injury or vascular incidents—are extremely rare but have been documented. This underscores the importance of ensuring that any intervention is appropriate for your specific health condition and carried out by a trained professional who can recognise contraindications and adapt their approach accordingly.
Safety Protocols in Practice
In the UK, practitioners adhere to stringent safety protocols designed to minimise risk and protect patient wellbeing. A thorough assessment precedes any manual therapy session, which includes taking a detailed medical history and performing physical examinations to rule out conditions where spinal mobilisation or manipulation may not be suitable. Continuous communication throughout the treatment ensures that the patient’s comfort and safety remain paramount. Practitioners are also trained in recognising warning signs that would necessitate immediate referral to a medical doctor.
Professional Standards and Regulation
The practice of manual therapy in Britain is governed by clear professional standards set forth by regulatory bodies such as the Chartered Society of Physiotherapy (CSP), the Health and Care Professions Council (HCPC), and other relevant organisations. These bodies provide comprehensive guidelines on ethical conduct, ongoing professional development, informed consent, and evidence-based practice. Only registered professionals with recognised qualifications are permitted to perform spinal mobilisation or manipulation, offering reassurance that treatments are delivered safely and competently.
Your Wellbeing at the Centre
Ultimately, your safety is always at the heart of quality care. By choosing a qualified practitioner who complies with UK standards and maintains open communication about potential risks and realistic outcomes, you can feel confident that your experience of spinal mobilisation or manipulation will be both safe and supportive.
6. Integrating Manual Therapy into Long-Term Care
Integrating spinal mobilisation and manipulation into long-term care requires a thoughtful and patient-centred approach, especially within the framework of the NHS’s holistic ethos. Rather than existing as isolated interventions, manual therapy techniques should be woven seamlessly into comprehensive management plans for individuals living with chronic musculoskeletal conditions.
Embracing Multidisciplinary Collaboration
One of the strengths of UK healthcare is its emphasis on teamwork. Physiotherapists, occupational therapists, GPs, nurses, and specialists all play vital roles in supporting patients with long-term spinal issues. Open communication between these professionals helps ensure that manual therapy is appropriately timed and aligned with other treatments, such as medication management, exercise programmes, and psychological support.
Practical Steps for Clinicians
- Assess each patient holistically—consider their physical health, mental wellbeing, social circumstances, and personal goals when recommending manual therapy.
- Document clear treatment objectives and regularly review progress in multidisciplinary meetings to adapt interventions as needed.
- Encourage shared decision-making, involving patients and carers in discussions about how manual therapy fits within their broader care plan.
Promoting Self-Management and Independence
Manual therapy can provide valuable relief and improve mobility, but it should be seen as one part of a larger strategy empowering individuals to manage their own health. Teaching patients gentle home exercises, posture strategies, and pain management techniques enhances the benefits of hands-on treatment while fostering independence—a key value in UK long-term care settings.
Ultimately, blending manual therapy with wider long-term condition management requires both clinical expertise and compassionate partnership. By working collaboratively and respecting each person’s unique journey, we honour the NHS commitment to holistic care—supporting not only the spine but the whole person over time.
7. Future Directions and Continuing Professional Development
As manual therapy continues to evolve within the UK, practitioners are encouraged to stay abreast of ongoing research and emerging best practices in spinal mobilisation and manipulation. The landscape of manual therapy is shaped by a commitment to evidence-based practice, patient safety, and person-centred care—values deeply rooted in the UK’s healthcare system.
Reflecting on Ongoing Research
Recent studies conducted across British universities and NHS trusts highlight the importance of integrating new scientific findings into clinical practice. Staying informed about these developments not only enhances treatment outcomes but also ensures that therapists can confidently address diverse patient needs. Participating in research projects or engaging with academic journals fosters a culture of inquiry and reflection, supporting lifelong learning.
Emerging Best Practices
With guidelines from reputable organisations such as the National Institute for Health and Care Excellence (NICE) and the Chartered Society of Physiotherapy (CSP), there is a growing emphasis on tailored interventions, shared decision-making, and safeguarding patient wellbeing. Practitioners are encouraged to adopt approaches that respect each individual’s unique health journey while drawing upon robust clinical frameworks.
Opportunities for Personal Growth
Pursuing continuing professional development (CPD) is both a regulatory requirement and an invaluable opportunity for personal growth. Attending workshops, enrolling in advanced training programmes, or joining peer supervision groups can strengthen both technical skills and reflective practice. In the spirit of gentle companionship, building supportive networks with colleagues creates space for open discussion, feedback, and encouragement.
Professional Learning within the UK Context
The UK’s rich tradition of professional standards provides a solid foundation for advancing knowledge and expertise. Engaging with local CPD events, online courses accredited by UK bodies, or multidisciplinary conferences allows therapists to broaden their perspectives while remaining sensitive to regional differences in service delivery.
Looking ahead, embracing change with curiosity and compassion will ensure that manual therapy practitioners continue to make meaningful contributions to patients’ lives. By nurturing a mindset of continuous learning and collaboration, we not only uphold the highest standards of care but also foster hope and resilience within our communities.