Introduction to Rehabilitation in the UK
Rehabilitation plays a pivotal role in supporting older adults across the United Kingdom, particularly those recovering from major injuries such as hip fractures. The process of rehabilitation encompasses a broad spectrum of services designed to help individuals regain independence, restore function, and improve quality of life after illness or injury. In the UK context, these services are primarily organised and delivered through the National Health Service (NHS), reflecting national health priorities and policy frameworks that emphasise equitable access and continuity of care. For older adults, especially those facing complex recovery journeys like hip fracture patients, rehabilitation is not merely about physical recovery but also involves psychological and social support tailored to individual needs. British health policy underscores the importance of timely intervention, multidisciplinary collaboration, and community integration, ensuring that every older adult has an opportunity to recover with dignity and autonomy. This introduction sets the stage for a deeper exploration of how rehabilitation pathways are structured within the NHS, highlighting their significance for the well-being of older people throughout the UK.
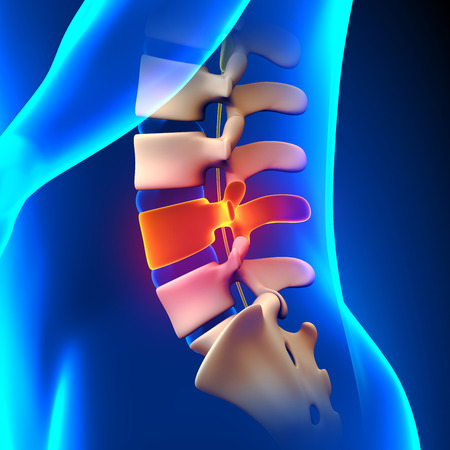
2. The Prevalence and Impact of Hip Fractures Among Older Adults
Hip fractures are a significant public health concern within the United Kingdom, particularly among the ageing population. As life expectancy continues to rise, so too does the incidence of hip fractures, creating a ripple effect that extends beyond the individual to families and the wider health and social care system.
Incidence of Hip Fractures in the UK
According to recent data, over 70,000 hip fractures occur each year in the UK, with the majority affecting people aged 65 and above. Women are disproportionately affected due to higher rates of osteoporosis post-menopause. The following table summarises key statistics:
| Age Group | Annual Incidence per 100,000 | Percentage of Total Cases |
|---|---|---|
| 65-74 | 260 | 18% |
| 75-84 | 830 | 42% |
| 85+ | 2,300 | 40% |
The Effects on Individuals and Families
The aftermath of a hip fracture can be life-changing. Many older adults experience a sudden loss of independence, mobility, and confidence. Rehabilitation is often lengthy and complex, with some never regaining their pre-injury level of function. This can lead to increased reliance on family members or carers for support with daily activities. Families frequently face emotional distress as well as practical challenges in providing ongoing care.
The Burden on Health Services
The NHS and associated social services bear a substantial burden from hip fractures. Hospital stays tend to be longer than average, and there is a high risk of complications such as infections or secondary falls. The cost implications are considerable: it is estimated that hip fractures cost the NHS over £1 billion annually when considering acute care, rehabilitation, and long-term support.
Summary Table: Impact Areas
| Stakeholder | Main Impact | Examples |
|---|---|---|
| Older Adult | Loss of independence; physical pain; reduced quality of life | Need for assistive devices; potential move to care home |
| Family/Carers | Increased caregiving responsibilities; emotional strain | Time off work; stress-related health issues |
| NHS & Social Care Services | Financial pressure; resource allocation challenges | Longer hospital stays; need for multidisciplinary teams |
The high prevalence and profound impact of hip fractures highlight the necessity for clear, effective rehabilitation pathways tailored to the needs of older adults in the UK context. Understanding these challenges is essential for designing interventions that not only address medical recovery but also support holistic wellbeing for patients and their families.
3. Acute Hospital Care and Initial Management
Upon arrival at Accident & Emergency (A&E) following a suspected hip fracture, older adults in the UK are rapidly assessed by the acute care team. The pathway typically begins with prompt pain management, radiological imaging to confirm diagnosis, and a multidisciplinary assessment to identify any immediate medical or surgical needs. Timeliness is critical; national guidelines such as those from NICE recommend that surgery should occur within 36 hours of admission if clinically appropriate.
Once admitted from A&E, patients are transferred to specialist orthopaedic or trauma wards. Here, the approach is fundamentally multidisciplinary. Consultant orthopaedic surgeons lead on surgical intervention, while anaesthetists ensure optimal perioperative care, especially for frail or comorbid patients. Geriatricians play a key role in assessing pre-existing health conditions and minimising post-operative complications—a practice codified in the Best Practice Tariff, which incentivises joint care between orthopaedics and geriatrics.
Beyond the operating theatre, physiotherapists and occupational therapists are involved early—often within 24 hours post-surgery—to initiate mobilisation and assess functional needs. Nurses specialised in orthopaedic or elderly care provide ongoing monitoring, wound management, and support with activities of daily living. Social workers may also be engaged to begin discharge planning even at this early stage, ensuring that longer-term rehabilitation pathways are considered from the outset.
Throughout acute hospital care, standards such as those set by the National Hip Fracture Database (NHFD) shape practice: these include regular multidisciplinary team meetings and adherence to evidence-based protocols for pain control, delirium prevention, pressure ulcer avoidance, and nutritional support. The clear aim is to maximise recovery potential while minimising complications during this crucial initial phase of hip fracture management in older adults across the UK.
4. Transitioning from Hospital to Community Care
For older adults recovering from a hip fracture in the UK, the transition from hospital to community care is a pivotal stage in the rehabilitation pathway. This phase is often complex, requiring meticulous discharge planning, close coordination with social care services, and robust communication between multidisciplinary teams. In this section, we examine the core elements of this transition and outline the common challenges faced by patients and their families.
Discharge Planning: A Multidisciplinary Approach
Effective discharge planning begins early during the hospital stay. The process typically involves a range of professionals including orthopaedic consultants, physiotherapists, occupational therapists, nurses, and social workers. Their collective goal is to assess the patient’s needs and determine the level of support required at home or within a community setting. The following table summarises key roles involved in discharge planning:
| Role | Main Responsibilities |
|---|---|
| Orthopaedic Consultant | Oversees medical management and surgical follow-up |
| Physiotherapist | Assesses mobility, develops exercise plans for recovery |
| Occupational Therapist | Evaluates home environment, recommends adaptations |
| Nurse | Coordinates care needs, provides education on medication and wound care |
| Social Worker | Liaises with community services, arranges ongoing social support |
Coordination with Social Care Services
The seamless integration of health and social care services is crucial for reducing hospital readmissions and promoting independence. Local authorities play a key role in assessing eligibility for funded support such as domiciliary care or adaptations to the home (e.g., grab rails, ramps). Joint care plans are often developed under frameworks like the Care Act 2014, ensuring that personal preferences and safety concerns are addressed.
Common Community Support Options:
- Domiciliary (home) care packages tailored to individual needs
- Reablement services aimed at regaining daily living skills over short periods (typically up to six weeks)
- Intermediate care beds within community hospitals or residential settings for those not yet able to return home safely
- Outpatient rehabilitation appointments for ongoing physiotherapy or occupational therapy input
Challenges During the Transition Phase
The transition from hospital to home can present several challenges unique to the British system:
- Delays in arranging community support: Pressures on local authority budgets and workforce shortages can result in extended hospital stays while awaiting suitable care packages.
- Communication gaps: Handover between NHS hospital teams and social care providers may be fragmented, leading to confusion about responsibilities or missed follow-ups.
- Patient and carer anxiety: Older adults and their families may feel uncertain about managing new equipment or medications without immediate professional support.
- Inequities in access: Rural areas or regions with limited services may face additional barriers compared to urban centres.
Towards Better Transitions: Best Practices Emerging in the UK
Pilot schemes such as ‘discharge-to-assess’ models—where assessments occur at home rather than in hospital—are gaining traction across various NHS Trusts. These initiatives aim to minimise unnecessary delays, improve patient satisfaction, and make more efficient use of acute beds. Consistent use of electronic health records also supports better information sharing between agencies involved in post-discharge care.
5. Community Rehabilitation Pathways and Support
Successful recovery from a hip fracture for older adults in the UK hinges not only on acute hospital care, but also on the ongoing support available within the community. This phase is critical, as it addresses both physical and social aspects of rehabilitation, aiming to restore independence and quality of life.
Physiotherapy Services
Community-based physiotherapy is a cornerstone of post-discharge care. NHS trusts typically offer structured programmes focusing on strength, balance, and mobility to help individuals regain functional movement. Sessions may occur in local health centres or at home, depending on the patients needs and circumstances. Importantly, these interventions are tailored to each individual’s progress, ensuring that goals remain realistic and achievable.
Occupational Therapy
Occupational therapists play a vital role in helping older adults adapt their living environments and routines following a hip fracture. Assessments often focus on daily tasks such as washing, dressing, cooking, and safe use of stairs. Recommendations might include adaptive equipment—like grab rails or perching stools—and strategies to reduce fall risk at home.
Reablement Services
Reablement services, typically arranged through local authorities, provide short-term intensive support aimed at promoting independence after hospital discharge. These time-limited interventions involve multi-disciplinary teams who work closely with patients to rebuild confidence and skills needed for daily living. The emphasis is firmly on enabling people to do things for themselves rather than doing things for them.
Support from Local Authorities and Voluntary Sector Organisations
Beyond NHS services, local councils may offer additional support such as personal care assistance, home adaptations, or telecare solutions. Furthermore, voluntary sector organisations—including Age UK and the Royal Voluntary Service—provide befriending schemes, transport to appointments, exercise classes, and peer support groups. These resources can make a tangible difference to mental wellbeing and social connectedness during recovery.
A Collaborative Approach
The community rehabilitation landscape in the UK is characterised by close collaboration among health professionals, local authorities, voluntary agencies, and families. Regular communication ensures that evolving needs are met promptly and holistically. As pathways vary by region, it is important for patients and carers to seek guidance from GPs or hospital discharge teams about what local resources are available.
Key Takeaway
Ongoing rehabilitation in the community forms an essential part of the hip fracture recovery journey for older adults in the UK. Harnessing physiotherapy, occupational therapy, reablement services, and wider community support maximises opportunities for regaining independence and improving overall wellbeing.
6. Barriers and Enablers in the UK Context
Recovery from hip fracture in older adults is shaped by a complex interplay of social, economic, and systemic factors unique to the UK context. Understanding these barriers and enablers is crucial for optimising rehabilitation pathways and ensuring positive outcomes.
Social Factors
Social support plays a pivotal role in rehabilitation. Older adults living alone or with limited family involvement may struggle with mobility, medication management, and attending follow-up appointments. In contrast, those with strong networks—be it family, friends, or community groups—often have improved motivation and practical assistance, leading to better functional recovery.
Economic Considerations
Socio-economic status continues to be a significant determinant in access to high-quality rehabilitation services across the UK. Individuals from more deprived backgrounds may face challenges such as limited access to private physiotherapy, inability to afford home adaptations, or insufficient funds for transport to outpatient clinics. Conversely, patients with greater financial resources may benefit from additional care options that accelerate recovery.
Systemic Influences
The structure of the NHS ensures that all patients receive core rehabilitation services following a hip fracture. However, regional disparities in service provision persist due to local commissioning priorities and resource constraints. Waiting times for community-based physiotherapy or occupational therapy can vary significantly between regions, sometimes leading to delays in essential interventions.
Continuity of Care
Effective communication and coordination between hospital teams and community services are critical enablers for smooth transitions post-discharge. Fragmentation in care pathways—such as missed handovers or unclear rehabilitation plans—can hinder progress and increase the risk of readmission.
Cultural Attitudes
Attitudes towards ageing and independence influence both patient engagement and professional expectations. In some cases, low expectations regarding recovery potential in older adults can inadvertently limit the intensity or ambition of rehabilitation goals set by clinicians.
Conclusion: Addressing Barriers, Amplifying Enablers
A comprehensive approach that addresses social isolation, mitigates economic inequalities, and strengthens integrated care pathways is essential for improving rehabilitation outcomes after hip fracture among older adults in the UK. Recognising these multifaceted influences allows practitioners and policymakers alike to design targeted interventions that truly support older people on their journey to recovery.
7. Conclusion and Future Directions
The recovery journey for older adults following a hip fracture in the UK is shaped by a complex interplay of clinical, social, and systemic factors. Throughout this article, we have highlighted how timely multidisciplinary rehabilitation, early mobilisation, and seamless transitions between hospital and community settings are crucial for optimal outcomes. Despite the strengths of the NHS and local authorities in providing coordinated care, gaps remain in service consistency, access to specialist support, and tailored interventions for individuals with diverse needs.
Looking ahead, there are clear opportunities for innovation and improvement within British rehabilitation pathways. Embracing digital health tools—such as remote monitoring and virtual physiotherapy—could increase accessibility, especially for those in rural or under-resourced areas. Furthermore, expanding personalised care plans that account for pre-existing conditions and social circumstances would enhance recovery trajectories. Collaborative efforts across health and social care sectors, underpinned by robust data-sharing and integrated funding models, could further streamline patient experiences.
To ensure future pathways are fit for purpose, ongoing evaluation of existing programmes is essential. Engaging older adults and their families in service design will help embed lived experience into policy development. Ultimately, realising these improvements will require sustained investment, workforce training, and a commitment to equity across all regions of the UK. By focusing on these directions, we can build a more resilient and responsive system that truly supports older people through their hip fracture recovery journey.