1. Understanding the Back: Key Structures and Functions
The human back is a remarkable structure, quietly supporting us through every step and movement of daily life. At its core lies the spine, or vertebral column, which acts as both a sturdy pillar and a flexible spring. This intricate chain of bones—known as vertebrae—is separated by soft discs that cushion impact and allow for gentle movement. Surrounding the spine are layers of muscles, each working in harmony to stabilise posture and enable everything from lifting shopping bags to enjoying a gentle stroll in the park.
Nerves weave their way through this network, carrying messages between the brain and body. They help us feel sensations, control muscles, and react to our surroundings. When these structures function well together, they provide the foundation for comfort, mobility, and overall wellbeing. Yet, like any well-loved piece of machinery, our backs need care and understanding to keep them functioning at their best. By appreciating how each part contributes to our everyday lives, we can nurture our backs with greater awareness and kindness.
2. Common Causes of Back Pain in the UK
Back pain is an all-too-familiar companion for many people across the UK, affecting individuals from all walks of life. Understanding the common causes can help us take gentle steps towards prevention and healing. In Britain, several factors contribute to back discomfort, ranging from lifestyle habits to occupational risks and local patterns of injury.
Sedentary Lifestyles and Desk-based Work
With a growing number of Britons spending hours at desks or in front of screens, sedentary lifestyles have become a leading culprit in back pain prevalence. The shift towards remote working has further increased the time many spend seated, often without ergonomic support. Poor posture and lack of movement can strain the muscles and ligaments that support the spine, gradually leading to discomfort or even chronic issues.
Manual Labour and Occupational Hazards
The UK’s diverse workforce includes many who are engaged in manual labour—builders, healthcare workers, delivery drivers, and more. These jobs frequently involve lifting heavy objects, repetitive movements, or standing for long hours. Such activities can place significant stress on the lower back and increase the risk of acute injuries like sprains or herniated discs.
Local Examples of Common Back Injuries
| Occupation/Activity | Typical Injury | Prevalence in UK |
|---|---|---|
| Office Workers | Muscular Strain, Postural Pain | Very Common (especially in London & major cities) |
| Construction Workers | Lumbar Sprain, Disc Injury | Common in urban development areas |
| Nurses & Carers | Lifting-related Injuries | Frequent in NHS & care homes |
| Cyclists/Commuters | Repetitive Strain, Sciatica | Notable in larger cities with high cycling rates (e.g., Cambridge) |
The British Weather and Physical Activity Patterns
The famously unpredictable British weather also plays a subtle role. Cold and damp conditions may discourage outdoor activity, leading to stiffness and reduced mobility for some. Additionally, winter falls or slips on icy pavements can cause sudden back injuries, especially among older adults.
A Gentle Reminder: Individual Risk Factors Matter Too
While lifestyle and occupation are important triggers, individual factors—such as age, underlying health conditions, and fitness levels—also influence susceptibility to back pain. Recognising these common causes allows us to approach prevention and care with empathy and understanding tailored to our unique circumstances in the UK.
3. Frequent Injuries and Their Impact
Back pain is a common complaint among people in the UK, often resulting from a handful of frequent injuries that can significantly disrupt daily life. Understanding these injuries helps us to recognise symptoms early and seek appropriate care, while also fostering compassion for those living with ongoing discomfort.
Slipped Discs: The Hidden Agony
A slipped disc, sometimes called a prolapsed or herniated disc, occurs when the soft tissue between the bones in your spine pushes out. This can press on nearby nerves, leading to pain, numbness, or tingling that radiates down your arms or legs. Everyday activities—like sitting at your desk in the office, carrying shopping bags, or even just tying your shoes—can become daunting tasks. In severe cases, mobility may be affected, making it difficult to get through even the most basic routines without assistance.
Muscle Strains: The Common Culprit
Muscle strains are perhaps the most widespread cause of back pain in Britain, often arising from lifting heavy objects incorrectly, sudden movements, or prolonged poor posture (such as hunching over a computer at work). Symptoms include aching muscles, stiffness, and localised swelling. These strains might make it uncomfortable to walk, stand up straight, or even sleep well at night—impacting both physical independence and emotional wellbeing.
Sciatica: Nerve Pain That Travels
Sciatica refers to pain caused by irritation of the sciatic nerve, which runs from your lower back down through your legs. The hallmark is shooting pain that travels along this pathway, sometimes accompanied by pins and needles or weakness in one leg. British weather—with its cold dampness—can sometimes make these symptoms feel worse. Sciatica can restrict simple pleasures like gardening on weekends or enjoying a stroll in the park with loved ones.
The Emotional Toll
While these injuries each have unique physical symptoms, they share a common impact: they can limit participation in cherished daily activities and undermine independence. Many people experience frustration or sadness as their routines are disrupted. Its important to remember that these feelings are valid—and that support from family, friends, and health professionals plays a crucial role in recovery.
Supporting Recovery Together
Recognising the signs and understanding how back injuries affect everyday life encourages empathy and early intervention. With gentle encouragement and practical support—from helping with household chores to providing transport to physiotherapy appointments—we can help those suffering from back pain feel less isolated as they journey towards healing.
4. The Healing Process: How the Body Recovers
Understanding how the body heals after a back injury can provide both reassurance and guidance. The human body is remarkably resilient, equipped with natural mechanisms that support recovery, especially when given the right care and time. While it’s natural to feel worried during episodes of back pain, it helps to know that most cases improve significantly with a combination of rest, gentle movement, and familiar self-care routines.
The Body’s Natural Recovery Mechanisms
After an injury or strain, your body begins a series of healing responses. These include reducing inflammation, repairing damaged tissues, and gradually restoring strength and flexibility to the affected area. In the UK, it’s common practice to follow the advice of “keep moving if you can” – an approach supported by modern research that emphasises gentle activity over prolonged bed rest.
Stages of Healing
| Stage | What Happens | Typical Duration |
|---|---|---|
| Inflammation | The body increases blood flow to the injured area, which may cause swelling and discomfort. | Few days |
| Tissue Repair | Damaged muscles, ligaments, or discs begin to mend themselves as new tissue forms. | 1–3 weeks |
| Remodelling | The new tissue strengthens and adapts as normal movement is gradually resumed. | Several weeks–months |
Rest and Gentle Movement: Finding Balance
While rest is essential in the early days following a back injury, complete immobility can actually slow down recovery. In Britain, many people find comfort in short walks around their home or garden once the initial pain subsides. Gentle stretches – such as those recommended by local NHS physiotherapists – can help maintain mobility without aggravating symptoms.
Self-Care Routines Familiar in the UK
- Hot water bottles: Applying gentle heat to stiff muscles is a classic British remedy for easing discomfort.
- Mild over-the-counter pain relief: Paracetamol or ibuprofen can be helpful for managing soreness while remaining active.
- Pacing activities: Breaking tasks into manageable chunks is a sensible way to avoid overexertion.
- Mindful relaxation: Techniques such as mindfulness or listening to calming radio programmes like BBC Radio 4 can reduce tension and promote healing.
The journey through back pain is rarely linear, but with patience and supportive habits rooted in daily British life, most people see steady improvement. Remember: seeking advice from your GP or local physiotherapist ensures you’re on the right path for your unique needs.
5. Holistic Approaches for Recovery and Long-term Care
Living with back pain can be both physically and emotionally challenging, but a holistic approach rooted in compassion and evidence-based care can make a meaningful difference. In the UK, many individuals find comfort in combining NHS-recommended therapies with practical self-help strategies that fit into everyday British life.
Pain Management: Compassionate Guidance
Managing back pain often begins with gentle reassurance and patient understanding. The NHS advocates starting with simple analgesics such as paracetamol or ibuprofen, always following the guidance of your GP or pharmacist. For those who need extra support, prescribed medications may sometimes be considered, but it’s wise to use these under professional supervision to avoid dependency or side effects.
Physiotherapy: Movement and Rehabilitation
Physiotherapy remains a cornerstone of back pain recovery in the UK. NHS physiotherapists work collaboratively with patients, designing tailored exercise programmes that gradually restore mobility and strength. These sessions might include core strengthening, stretching routines, and education on posture—empowering you to regain confidence in your movements over time. Remember, consistency is key; even short daily exercises can yield significant improvements.
Self-Help Strategies for Everyday Life
Incorporating small yet impactful changes into your routine can greatly aid recovery. The British climate often means damp or chilly days—so keeping active indoors is essential. Activities such as gentle yoga or Pilates, readily available via online classes or local community centres, help keep muscles supple and spirits lifted. Regular walks in your local park or green space provide fresh air and gentle exercise without overstraining your back.
Mindful Living: Emotional Wellbeing
Caring for your mental health is just as important as tending to physical discomfort. Mindfulness practices, like deep breathing or guided meditation (many of which are offered by charities such as Mind), can help manage stress and reduce the emotional burden of chronic pain. Don’t hesitate to reach out to support groups or helplines if you need someone to talk to—community is a vital part of long-term healing.
Adapting Your Home and Work Environment
Practical adjustments around the house or at work can prevent further injury and support ongoing recovery. Consider investing in an ergonomic chair for your home office or using supportive cushions while watching telly. Take regular breaks from sitting—set a timer if needed—and use proper lifting techniques when handling shopping bags or household items.
By weaving together professional advice, compassionate self-care, and adaptations suited to British lifestyles, you can nurture both body and mind throughout your journey with back pain. Remember: healing is not always linear, but every small step counts toward better wellbeing.
6. When to Seek Professional Support
Understanding when to seek professional help for back pain is an essential part of self-care and long-term wellbeing. While many cases of back discomfort improve with rest, gentle exercise, and over-the-counter remedies, there are times when consulting a healthcare professional is not just wise but necessary. This guidance will gently walk you through recognising those moments and introduce you to the UK’s trusted resources for ongoing support.
Signs It’s Time to Consult Your GP
If your back pain persists beyond a few weeks, or if it interferes significantly with daily activities such as walking, sleeping, or working, it’s advisable to book an appointment with your GP. Other warning signs include:
- Pain that spreads down your legs or causes numbness and tingling
- Weakness in the legs or feet
- Unexplained weight loss alongside your back pain
- Pain following a serious injury, such as a fall or accident
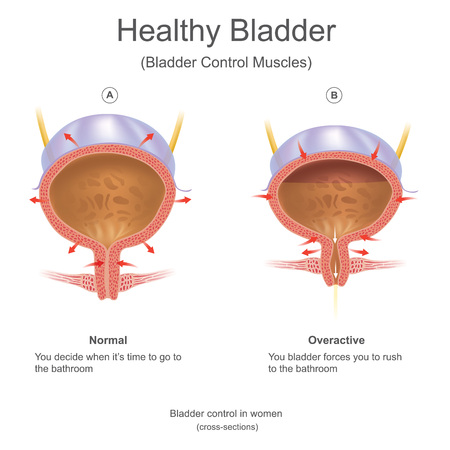
- Loss of bladder or bowel control (which requires urgent medical attention)
The NHS Pathway
The NHS provides comprehensive guidance on back pain management. Your GP may offer advice on lifestyle changes, prescribe medication, or refer you for physiotherapy. In some cases, you may be referred to a specialist—such as an orthopaedic consultant or a pain clinic—particularly if conservative treatments haven’t helped.
Accessing Local Resources
You can find more information on the NHS website, where you’ll discover self-help tips and details about local services. Many regions also have dedicated musculoskeletal clinics that accept NHS referrals for persistent or complex cases.
Ongoing Support for Chronic Back Pain
If you’re living with long-term back pain, organisations like Versus Arthritis and BackCare UK offer helplines, peer support, and educational materials tailored to the British experience. These resources can provide reassurance and community as you navigate your healing journey.
Remember: seeking timely professional advice is a positive step towards recovery and maintaining your independence. The UK’s supportive healthcare framework ensures you’re never alone in managing back pain—gentle guidance and practical solutions are always within reach.


