Introduction to Chronic Pain and Postural Issues
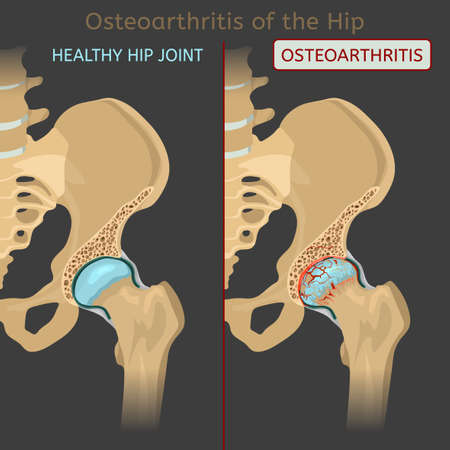
Chronic pain represents a significant public health concern across the United Kingdom, affecting an estimated one in five adults. This persistent discomfort—often defined as pain lasting longer than twelve weeks—can have a profound impact on daily life, limiting mobility, reducing participation in work and social activities, and diminishing overall quality of life. The economic burden is equally considerable, with chronic musculoskeletal conditions being among the leading causes of long-term sickness absence in the UK workforce.
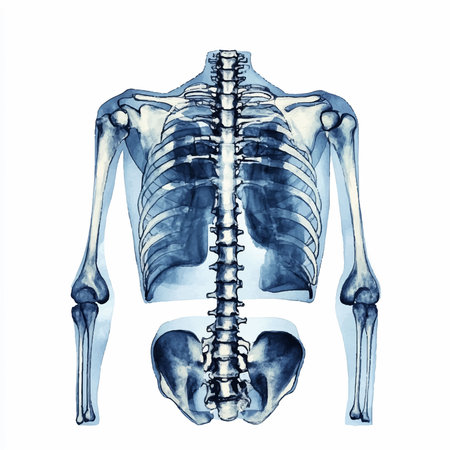
Among the various contributors to chronic pain, postural factors are frequently identified as both causative and perpetuating elements. In the British context, where sedentary lifestyles and desk-based occupations are commonplace, poor posture has become increasingly prevalent. Common postural issues such as forward head carriage, rounded shoulders, and excessive lumbar lordosis are known to place undue strain on muscles, ligaments, and joints. Over time, these maladaptive patterns can lead to persistent pain syndromes affecting the neck, back, shoulders, and lower limbs.
Understanding the interplay between postural alignment and chronic pain is crucial for effective management strategies. British physiotherapy protocols emphasise a holistic approach that addresses not only the symptoms but also the underlying biomechanical dysfunctions contributing to longstanding discomfort. By recognising the widespread impact of chronic pain and its strong association with postural habits, healthcare professionals in the UK are better equipped to design targeted interventions aimed at restoring function and improving patients’ quality of life.
2. British Approaches to Postural Assessment
The assessment of posture forms a cornerstone in the management of chronic pain within British physiotherapy practice. Guided by the National Institute for Health and Care Excellence (NICE) guidelines, UK physiotherapists employ a structured and evidence-based approach to postural assessment, ensuring interventions are both safe and effective. The process is not only clinical but also holistic, taking into account individual patient circumstances and broader health determinants.
Standard Assessment Tools in the UK
British physiotherapists utilise a combination of observational methods, validated screening tools, and digital technologies to assess postural deviations that may contribute to chronic pain. The following table summarises commonly employed tools and their respective uses:
| Assessment Tool | Description | Application in Practice |
|---|---|---|
| Visual Posture Analysis | Systematic visual inspection from multiple planes | Baseline identification of asymmetries and abnormal alignments |
| Photographic Analysis | Use of standardised photographs or video recordings | Objective documentation; progress tracking over time |
| Plumb Line Assessment | Comparison against anatomical landmarks with a vertical reference line | Detection of deviations from ideal posture in standing alignment |
| Postural Grids/Charts | Grid overlays for visual comparison and measurement | Enhanced accuracy in noting positional discrepancies |
| Validated Questionnaires (e.g., Oswestry Disability Index) | Patient-reported outcome measures focusing on function and pain impact | Integration of subjective experience with objective findings |
| Functional Movement Screens | Observation of dynamic tasks (e.g., sit-to-stand, gait) | Identification of movement patterns contributing to pain syndromes |
| Digital Posture Apps & Motion Analysis Systems | Technology-driven quantification of joint angles and segment positions | Differentiation of subtle abnormalities; data for audit/research purposes |
NICE Guidelines and Best Practice Integration
The NICE guidelines emphasise individualised assessment, advocating for a biopsychosocial model that recognises physical, psychological, and social factors influencing chronic pain. British best practice dictates that assessment should be collaborative, involving the patient’s goals and preferences while maintaining rigorous documentation standards. Importantly, any identified postural issues are contextualised within the patient’s lifestyle, occupation, and daily activities—core tenets underpinning UK healthcare delivery.
The Role of Interdisciplinary Communication
A distinctive feature in the British approach is strong interdisciplinary communication. Physiotherapists frequently collaborate with GPs, occupational therapists, and pain specialists to ensure postural findings inform broader management plans. This collaborative ethos aligns with NHS priorities for integrated care.
Summary Table: Key Elements in British Postural Assessment Practice
| Element | Description/Role |
|---|---|
| NICE-Informed Protocols | Ensure assessments are evidence-based and standardised across settings. |
| Holistic Patient Involvement | Engagement with patients lived experience for tailored interventions. |
| Objective & Subjective Measures Combined | Blends clinical observation with patient self-reporting tools. |
| Regular Review & Reassessment | Keeps intervention responsive to changes in posture or pain status. |
This comprehensive, structured methodology enables British physiotherapists to develop precise postural correction strategies that are both clinically robust and sensitive to the complexities of chronic pain management within the UK context.
3. Key Principles of Postural Correction
Alignment: The Foundation of Effective Posture
British physiotherapy protocols emphasise that optimal postural alignment forms the cornerstone of chronic pain management. Correct alignment involves maintaining the natural curves of the spine—cervical, thoracic, and lumbar—while standing or sitting. Physiotherapists employ evidence-based assessment tools to analyse deviations from ideal posture, such as forward head carriage or excessive lumbar lordosis. Through targeted interventions, patients are guided to achieve neutral spinal positions, which alleviate undue stress on muscles and joints, thereby reducing chronic discomfort. Regular reassessment ensures that improvements in alignment translate into long-term pain relief.
Ergonomics: Adapting Environments for Sustainable Change
Another key element within British protocols is ergonomics—the adaptation of living and working environments to support correct posture. Physiotherapists conduct thorough ergonomic assessments, often in collaboration with occupational health teams, to identify risk factors in patients’ daily routines. Recommendations may include adjusting chair height, screen positioning, or introducing lumbar supports. These evidence-based modifications help mitigate the cumulative strain associated with sedentary lifestyles or repetitive tasks, which are prevalent contributors to musculoskeletal pain in the UK workforce.
Education: Empowering Self-Management
Patient education is integral to all British postural correction strategies. Physiotherapists deliver tailored advice on body mechanics, safe movement patterns, and the importance of regular activity breaks. Educational sessions often utilise visual aids and practical demonstrations to enhance understanding and adherence. By fostering patient awareness and self-monitoring skills, British practitioners empower individuals to take an active role in their own pain management journey.
Evidence-Based Approach
All interventions adhere strictly to evidence-based guidelines issued by reputable bodies such as the Chartered Society of Physiotherapy (CSP) and National Institute for Health and Care Excellence (NICE). This ensures that recommended postural correction techniques are both clinically effective and culturally relevant for the UK population.
Summary
The British approach to postural correction for chronic pain incorporates precise alignment strategies, ergonomic adaptations, and comprehensive education—all grounded in robust clinical evidence. This multidimensional method not only addresses existing pain but also equips patients with lifelong skills for prevention and self-care.
4. Therapeutic Exercise and Rehabilitation
Therapeutic exercise and rehabilitation form the cornerstone of postural correction within British physiotherapy protocols, especially for managing chronic pain. UK-based physiotherapists apply evidence-based exercise regimes, tailored movement strategies, and hands-on interventions to address both the underlying biomechanical dysfunctions and their symptomatic manifestations. This section explores the most prevalent practices adopted across NHS and private clinics in Britain.
Common Exercise Regimes in the UK
Physiotherapists in the UK commonly prescribe a combination of stretching, strengthening, and mobility exercises aimed at restoring musculoskeletal balance. The focus is often on muscle groups that contribute to poor posture—such as weakened core stabilisers or tight hip flexors—and on facilitating neuromuscular re-education. A typical protocol may include:
| Exercise Type | Purpose | Example Exercises |
|---|---|---|
| Stretching | Lengthen tight muscles limiting posture | Hamstring stretch, chest opener |
| Strengthening | Enhance support from weak muscles | Pilates-based core work, glute bridges |
| Mobility Training | Improve joint range of motion | Thoracic rotations, dynamic lunges |
| Balance/Proprioception | Refine movement control and stability | Single-leg stands, wobble board exercises |
Movement Strategies Employed by British Physiotherapists
Apart from exercise prescription, British physiotherapists emphasise patient education in daily ergonomics and self-management techniques. Movement retraining is integral; patients are guided to modify habitual patterns such as sitting, standing, and lifting—thereby reducing mechanical stress on vulnerable structures. Common cues include:
- Sitting with neutral spine alignment using lumbar supports
- Standing with weight evenly distributed over both feet
- Lifting with a straight back and engaging the lower limbs rather than the spine
- Taking regular breaks from static postures during work or leisure activities
Physiotherapy Interventions: Manual Therapy and Modalities
While therapeutic exercise remains primary, hands-on interventions are frequently integrated into British protocols to optimise outcomes. These may involve soft tissue mobilisation, joint manipulation (where indicated), taping techniques for proprioceptive feedback, and modalities such as ultrasound or TENS for pain modulation. The combination of manual therapy with active rehabilitation is widely supported by UK clinical guidelines.
NHS versus Private Practice Approaches
The NHS typically provides structured group classes (e.g., Back Care Programmes) alongside individualised care. Private practitioners may offer more bespoke one-to-one sessions with access to advanced technologies or Pilates equipment. Nevertheless, both sectors adhere to best-practice standards outlined by professional bodies like the Chartered Society of Physiotherapy (CSP).
Summary Table: Key Elements in UK Postural Rehabilitation Protocols
| Component | Description/Goal |
|---|---|
| Therapeutic Exercise | Treat muscular imbalance and restore function via targeted routines |
| Education & Self-Management | Empower patients to maintain corrections outside clinic settings |
| Manual Therapy & Modalities | Reduce pain and facilitate better movement through skilled interventions |
| Progressive Monitoring & Review | Regular assessment ensures ongoing adaptation to patient progress and needs |
This integrated approach epitomises contemporary British physiotherapy for chronic pain management—combining structured exercise regimes, strategic movement retraining, and adjunctive therapies for sustainable postural correction.
5. Patient Engagement and Self-Management
Empowering Patients within the NHS Framework
A cornerstone of effective postural correction for chronic pain management in the United Kingdom is a strong emphasis on patient engagement, particularly within the context of the NHS. British physiotherapy protocols prioritise shared decision-making, recognising that active participation by patients leads to improved outcomes and greater satisfaction. Physiotherapists routinely involve patients in goal setting, treatment planning, and progress monitoring, ensuring interventions are tailored to individual lifestyles and preferences.
Self-Management Techniques for Long-Term Success
Promoting self-management is vital for sustainable improvements in posture and pain reduction. NHS physiotherapists teach patients practical strategies such as regular posture checks, ergonomic adjustments at home and work, and simple stretching or strengthening exercises that can be incorporated into daily routines. These techniques foster independence and enable individuals to take ownership of their rehabilitation journey beyond the clinical environment.
The Role of Patient Education
Education underpins every aspect of British physiotherapy practice. Patients are provided with clear information about the link between poor posture and chronic pain, including personalised advice on how specific lifestyle factors—such as prolonged sitting or repetitive movements—contribute to their symptoms. Educational materials may include leaflets, online resources, or group workshops designed to demystify musculoskeletal health and empower informed choices.
Utilising Community Resources
Community-based support is increasingly recognised as a valuable adjunct to formal NHS services. Local initiatives such as walking groups, exercise classes tailored for those with musculoskeletal conditions, or peer-led support networks offer ongoing encouragement and accountability. Physiotherapists often signpost patients to these resources, helping bridge the gap between structured therapy sessions and independent self-care in everyday life.
By integrating patient engagement strategies, self-management techniques, robust education programmes, and community resources, British physiotherapy protocols create a supportive framework that enables individuals to manage chronic pain proactively while fostering resilience and long-term wellbeing.
6. Case Studies and Clinical Outcomes
To illustrate the practical application and measurable benefits of British physiotherapy protocols for postural correction in chronic pain management, this section presents representative case studies from UK clinical settings. These examples highlight how structured interventions can lead to significant improvements in patient outcomes, reinforcing the value of evidence-based practice within the NHS framework.
Case Example 1: Office Worker with Chronic Lower Back Pain
A 42-year-old office worker from Manchester presented with persistent lower back pain attributed to prolonged sedentary work and poor ergonomic habits. Following a comprehensive assessment by a Chartered Physiotherapist, a tailored protocol was implemented, including ergonomic modifications, postural retraining exercises such as lumbar stabilisation, and education on regular movement breaks. After eight weeks, the patient reported a 60% reduction in pain on the Visual Analogue Scale (VAS), improved spinal alignment observed through follow-up postural analysis, and enhanced functional capacity documented via the Oswestry Disability Index.
Case Example 2: Retired Teacher Experiencing Chronic Neck Pain
A 65-year-old retired teacher from Bristol suffered from chronic neck discomfort associated with forward head posture. British physiotherapy protocols were applied, focusing on deep cervical flexor strengthening, scapular stability exercises, and integration of mindfulness-based postural awareness. Over a three-month period, the patient demonstrated improved cervical range of motion, reduced reliance on analgesics, and increased confidence in daily activities as measured by the Neck Disability Index (NDI). Patient-reported outcomes also indicated greater overall well-being and quality of life.
Case Example 3: Young Athlete Recovering from Recurrent Shoulder Pain
An 18-year-old amateur swimmer in London experienced recurrent shoulder pain linked to poor scapulothoracic control. The physiotherapy team employed a protocol involving corrective taping techniques, progressive resistance training targeting postural muscles, and biomechanical education specific to swimming technique. After twelve weeks, objective measures showed restored shoulder function (as per the Constant-Murley Score) and a marked reduction in pain during both training and competitions.
Clinical Implications
These case studies underscore the adaptability of British physiotherapy protocols across diverse age groups and occupational backgrounds. Each intervention was grounded in robust assessment tools and guided by clinical reasoning that aligns with current NICE guidelines. Notably, consistent monitoring using validated outcome measures facilitated objective evaluation of progress and informed ongoing treatment adjustments.
Conclusion
The outlined clinical cases demonstrate that postural correction strategies rooted in British physiotherapy practice offer tangible benefits for individuals living with chronic pain. Through patient-centred care pathways, measurable outcomes are achieved not only in symptom relief but also in functional restoration and self-management skills—hallmarks of effective long-term pain management within the UK health context.