Introduction: Navigating Arthritis Care in the UK
Arthritis is one of the most prevalent long-term health conditions in the UK, affecting over 10 million people and making it a significant public health concern. Whether it manifests as osteoarthritis, rheumatoid arthritis, or one of the many other forms, arthritis can profoundly impact mobility, independence, and overall quality of life. The journey towards recovery or effective management often requires a multifaceted approach, drawing on both medical intervention and rehabilitation support. In the UK, individuals typically begin their care pathway within the NHS, where GPs play a central role in diagnosis and initial management. However, as waiting lists for specialist appointments and physiotherapy continue to grow, many people are now exploring private rehabilitation options to supplement their NHS care. This landscape creates unique challenges—and opportunities—for those seeking to bridge NHS services with private sector solutions for optimal arthritis recovery.
2. The NHS Approach to Arthritis Management
In the UK, the National Health Service (NHS) is often the first port of call for individuals experiencing symptoms of arthritis. Understanding the NHS approach to arthritis management is key to appreciating both its strengths and limitations—especially when considering a bridge between public and private rehabilitation options.
Diagnosis and Initial Care Pathways
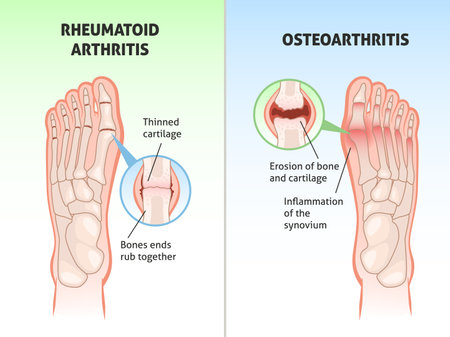
The NHS typically begins with a GP (General Practitioner) consultation, where initial assessments are made based on symptoms, medical history, and physical examination. If arthritis is suspected, patients may be referred for blood tests or imaging such as X-rays or MRI scans. Early diagnosis is crucial, particularly for inflammatory types like rheumatoid arthritis.
Standard NHS Care Pathway for Arthritis
| Stage | Key Steps | Typical Waiting Time |
|---|---|---|
| GP Consultation | Symptom assessment, referral if needed | Within 1-2 weeks |
| Specialist Referral | Appointment with rheumatologist or orthopaedic specialist | Up to 18 weeks (NHS target) |
| Diagnosis & Tests | Blood tests, imaging, clinical review | Varies, but often several weeks after referral |
| Treatment Initiation | Medication, advice on lifestyle changes, physiotherapy referral if indicated | Soon after diagnosis confirmed |
| Ongoing Management | Follow-ups with multidisciplinary team: nurses, physios, occupational therapists, pharmacists | Regular intervals as per care plan |
The Role of Multidisciplinary Teams (MDT)
A core strength of the NHS is its focus on holistic care through multidisciplinary teams. These teams bring together expertise from various healthcare professionals:
- Rheumatologists: Oversee complex cases and advanced medication management.
- Physiotherapists: Deliver tailored exercise programmes and mobility strategies.
- Occupational Therapists: Advise on adaptive techniques and equipment for daily living.
- Nurse Specialists: Provide patient education and ongoing support.
- Pharmacists: Monitor medication interactions and adjustments.
NHS Strengths and Challenges in Arthritis Care
| Strengths | Challenges |
|---|---|
| No direct cost at point of use Comprehensive MDT support Structured care pathways Access to evidence-based treatments |
Long waiting times for specialists Resource constraints limiting rehab intensity Shortage of consistent follow-up Limited access to cutting-edge therapies in some regions |
A British Perspective on Accessing NHS Services
The NHS remains a lifeline for many living with arthritis in the UK. However, the reality is that waiting lists can be lengthy—particularly for non-urgent referrals or specialist-led rehabilitation. This means some people seek complementary support from private providers to bridge gaps in their recovery journey. Recognising these realities is the first step towards integrating both sectors for optimal patient outcomes.
![]()
3. Limitations and Challenges in NHS Provision
When it comes to arthritis recovery, the NHS is often the first port of call for most people in the UK. However, despite its commitment to accessible healthcare for all, patients frequently encounter several hurdles that can impact their rehabilitation journey. One of the most commonly cited issues is the lengthy waiting lists for specialist services. It’s not unusual for individuals to wait weeks or even months before getting an appointment with a physiotherapist or rheumatology consultant. This delay can be incredibly frustrating, especially when you’re eager to start your recovery and prevent further joint deterioration.
Time constraints within NHS appointments also present a significant challenge. Most sessions with NHS therapists are limited to 20 or 30 minutes, which barely scratches the surface when you’re dealing with complex arthritis symptoms and need tailored guidance. These short slots often mean that ongoing support and in-depth education about self-management strategies are limited, leaving patients feeling under-supported once they leave the clinic.
Access to specialist rehabilitation is another barrier many people face. In some areas, there simply aren’t enough resources or trained professionals to meet demand—particularly for advanced therapies such as hydrotherapy or multi-disciplinary clinics. This postcode lottery means that where you live can dramatically affect the type and quality of arthritis care you receive through the NHS. For those wanting more than basic pain management advice, this can create a real sense of helplessness and prompt the search for alternatives outside of public healthcare.
4. Private Rehabilitation Options: A Complementary Solution
When discussing arthritis recovery in the UK, its vital to recognise that private rehabilitation services can play a crucial complementary role alongside NHS provisions. While the NHS offers foundational care and essential support, private rehab brings flexibility, quicker access, and tailored programmes that can significantly benefit those navigating arthritis recovery.
Availability of Private Rehabilitation Services
Private rehabilitation clinics are widely available across the UK, from major cities like London and Manchester to smaller towns. Many operate independently or as part of larger healthcare networks. Some focus exclusively on musculoskeletal and rheumatological conditions, while others provide broader physiotherapy and occupational therapy services. This variety ensures that most patients can access a suitable service within a reasonable distance, either in-person or through remote consultations.
Scope of Services Offered
The scope of private rehabilitation is often more expansive than what’s typically available on the NHS. Patients may benefit from:
- Bespoke physiotherapy sessions with flexible scheduling
- Advanced pain management techniques (e.g., acupuncture, hydrotherapy)
- Multi-disciplinary team input, including specialist consultants
- Access to cutting-edge equipment and facilities
- Comprehensive education on self-management strategies
Comparison Table: NHS vs. Private Rehabilitation Options
| Aspect | NHS | Private Rehabilitation |
|---|---|---|
| Waiting Time | Weeks to months | Usually days |
| Session Length & Frequency | Standardised; limited number | Flexible; as required by patient needs |
| Treatment Personalisation | Guidelines-based care | Highly individualised plans |
| Specialist Access | Referral dependent; may be limited | Direct booking; wider choice of experts |
| Add-on Therapies (e.g., Pilates, Hydrotherapy) | Limited availability | Broad range offered as standard or optional extras |
| Cost to Patient | No direct cost (funded by NHS) | Paid out-of-pocket or via insurance/health plans |
The Distinct Benefits for UK Patients
The biggest draw of private rehabilitation is its patient-centred approach. Those with arthritis often need ongoing support that adapts as their condition changes—private providers are well-placed to offer this continuity without long waits or rigid appointment structures. Additionally, many find value in receiving immediate feedback and being able to access therapies not readily available through public channels.
This doesn’t mean private rehab is a replacement for NHS care; instead, it fills gaps and empowers patients with greater choice and agency over their recovery journey. For those who can invest in these services—either personally or via employer health schemes—the potential for improved outcomes and enhanced quality of life is clear.
5. Bridging the Gap: Integrative Care Pathways
For many UK arthritis patients, making the most of both NHS services and private rehabilitation is not just about access—its about building a seamless journey towards recovery. Here are some practical strategies to help you bridge this gap effectively:
Shared Medical Records: Ensuring Continuity
One of the biggest hurdles is ensuring that your medical information flows smoothly between NHS and private providers. Patients can request copies of their records from their GP or hospital specialist and share these directly with private practitioners. Some private clinics now offer to liaise with your NHS team (with your consent), creating a unified care plan. This step is crucial in preventing duplicated tests, conflicting advice, and gaps in treatment.
Referrals: Navigating Both Worlds
While NHS GPs typically provide referrals within the NHS system, you are entitled to ask for a referral letter for private rehabilitation if you believe it will benefit your recovery. Be proactive—explain your goals and the type of therapy or expertise you seek. Conversely, reputable private clinicians can write back to your NHS GP with updates on your progress, which helps keep all parties aligned on your care pathway.
Financial Considerations: Making Informed Choices
The cost of private rehabilitation can be significant, but there are ways to make it more manageable. Some health insurance policies, including those provided by employers, cover part or all of private physiotherapy or occupational therapy costs—always check your policy details carefully. If self-funding, consider asking about package rates or payment plans offered by private clinics. Also, bear in mind that some charities and local council schemes offer grants or subsidies for arthritis-related rehabilitation.
Practical Tips for Navigating Care
– Keep a personal health journal to track symptoms, treatments, and questions for each provider.
– Use NHS online services like the NHS App to manage appointments and access test results.
– Build relationships with both your NHS GP and any private therapists—clear communication is key.
– Don’t hesitate to ask both sides how they can work together for your benefit.
By taking these steps, UK arthritis patients can create an integrative pathway that harnesses the strengths of both public and private sectors—maximising recovery potential while staying informed and empowered every step of the way.
6. Lived Experience: Real Stories of Arthritis Recovery
When it comes to bridging NHS services and private rehabilitation for arthritis recovery in the UK, nothing speaks louder than real-life experiences. Many people facing arthritis find themselves navigating a complex path—balancing what’s available through the NHS and seeking additional support from private providers. Here, we share a few personal accounts that highlight both the challenges and triumphs of this journey.
Sarah’s Journey: Finding the Right Balance
Sarah, a 54-year-old from Manchester, was diagnosed with rheumatoid arthritis three years ago. Initially, she relied entirely on her local NHS rheumatology clinic for treatment and physiotherapy. “The NHS team was brilliant,” Sarah recalls, “but I felt I needed more one-on-one sessions to really get my mobility back.” After some research and speaking with her GP, she decided to supplement her care with private hydrotherapy sessions. “Combining both services gave me not just better movement, but also confidence. The NHS supported me medically while the private rehab helped me tailor exercises to my daily routine.”
Tom’s Perspective: Overcoming Waiting Times
Tom, a retired teacher from Bristol, faced long waiting lists for NHS physiotherapy after his knee replacement surgery due to osteoarthritis. “The NHS did their best, but there was only so much they could do with the resources they had,” Tom says. He opted for a short-term package with a local private rehabilitation centre, focusing on intensive strength training. “It wasn’t cheap, but being able to move around without pain again made it worth every penny. I still go back to my NHS consultant for check-ups.”
Priya’s Story: Holistic Support
Priya, in her late thirties and living in London, describes her recovery as a partnership between NHS professionals and private specialists. “The NHS provided essential diagnostics and medication management,” she explains. “But when it came to diet advice and mental health support, I found a private rehab service that offered everything under one roof—from occupational therapy to nutritional counselling.” Priya credits this combined approach for helping her return to work and regain independence.
The Takeaway: Learning from Lived Experience
These stories underline an important reality: there is no one-size-fits-all solution for arthritis recovery in the UK. Many patients benefit from using both NHS and private rehabilitation services—sometimes out of necessity, sometimes by choice. The key is open communication with your healthcare team and being proactive about exploring all available options. Whether you’re making decisions about physiotherapy, pain management or lifestyle changes, learning from others’ journeys can help guide your own path towards recovery.
7. Empowering Your Recovery: Practical Tips and Resources
Taking charge of your arthritis recovery is entirely possible when you combine the strengths of both NHS services and private rehabilitation options available in the UK. Here’s how you can make the most out of this blended approach:
Know Your Entitlements and Take Initiative
Start by understanding what support you are entitled to through the NHS—this includes GP referrals, physiotherapy, occupational therapy, and specialist consultations. Don’t hesitate to ask your GP for a detailed care plan or to be referred for extra support if your needs change. If you feel your progress has plateaued, request a review or second opinion. Remember, being proactive is key within the NHS system.
Mix and Match Rehabilitation Options
If waiting lists are long or you need more intensive therapy, consider supplementing NHS care with private sessions. Look for local clinics accredited by reputable bodies like the Chartered Society of Physiotherapy (CSP) or British Association of Occupational Therapists (BAOT). Many private providers now offer hybrid packages tailored to people who are already receiving NHS support—this can save money and ensure continuity of care.
Seek Out Community-Based Support
The UK has a vibrant network of charities and support groups dedicated to arthritis. Organisations such as Versus Arthritis, Arthritis Action, and local Arthritis Care groups provide peer support, exercise classes, pain management workshops, and practical advice. Many run online forums where you can share experiences and tips with others on a similar journey.
Practical Steps You Can Take Today
- Use the NHS Service Finder to locate nearby services and check waiting times.
- Ask your GP about joint NHS-private care options—some areas have pilot schemes for combined pathways.
- Contact Versus Arthritis for guidance on rights at work, benefits, and self-management courses.
- Attend local arthritis-friendly exercise classes—many community leisure centres offer discounted rates for those with chronic conditions.
- Join a UK-based arthritis Facebook group or online forum to access real-time advice from people living with similar challenges.
Your Recovery, Your Way
No two recovery journeys look exactly alike. By leveraging both NHS resources and reputable private rehabilitation options—and plugging into supportive communities—you put yourself in the strongest position possible for long-term management and meaningful progress. Stay curious, keep asking questions, and remember: empowered patients get better results.