Introduction to Electrotherapy in Sports Injury Rehabilitation
Electrotherapy has steadily become an integral component of sports injury rehabilitation across the UK, reflecting both advances in technology and an evolving understanding of best practice in physiotherapy. At its core, electrotherapy refers to a collection of treatments that utilise electrical energy to manage pain, stimulate muscles, promote healing, and support functional recovery following musculoskeletal injuries. The principles behind these modalities are rooted in the application of controlled electrical currents to specific tissues, aiming to enhance the bodys natural repair processes while reducing discomfort for the patient. In recent years, British sports medicine practitioners have increasingly embraced electrotherapy due to its non-invasive nature and its ability to complement traditional approaches such as manual therapy and exercise-based rehabilitation. With a growing body of clinical evidence supporting its efficacy, electrotherapy now plays a vital role within multidisciplinary teams working with athletes at all levels—from grassroots community clubs through to elite sporting institutions—helping individuals recover more quickly and return safely to their chosen activities.
2. Common Electrotherapy Modalities Used in the UK
Within British physiotherapy settings, several electrotherapy modalities are regularly employed to support the rehabilitation of sports injuries. The most frequently utilised techniques include Transcutaneous Electrical Nerve Stimulation (TENS), therapeutic ultrasound, and interferential therapy. Each modality has its own unique application, evidence base, and clinical considerations, which make them suitable for different stages and types of sports-related injuries.
TENS (Transcutaneous Electrical Nerve Stimulation)
TENS is widely used across the UK as a non-invasive method for managing both acute and chronic pain associated with musculoskeletal injuries. By delivering mild electrical impulses through the skin, TENS aims to modulate pain signals and promote comfort during recovery. In British clinics, TENS machines are often recommended as part of home-based rehabilitation programmes, reflecting a patient-centred approach to long-term recovery and self-management.
Therapeutic Ultrasound
Therapeutic ultrasound is another staple in UK physiotherapy practice, particularly valued for its role in promoting tissue healing and reducing inflammation. High-frequency sound waves are applied to injured tissues, enhancing local blood flow and encouraging cellular repair processes. This modality is commonly indicated for soft tissue injuries such as ligament sprains, muscle strains, and tendonitis—conditions frequently seen in British sporting populations.
Interferential Therapy
Interferential therapy involves the use of two medium-frequency electrical currents that intersect within the affected tissue, resulting in deeper stimulation compared to TENS. It is particularly favoured by UK physiotherapists for its effectiveness in managing pain, swelling, and improving joint mobility. Interferential therapy often forms part of comprehensive rehabilitation plans for athletes recovering from more complex or persistent injuries.
Comparison of Common Electrotherapy Modalities in the UK
| Modality | Main Application | Typical Indications | Setting |
|---|---|---|---|
| TENS | Pain relief | Acute & chronic musculoskeletal pain | Clinic & home use |
| Ultrasound | Tissue healing & inflammation reduction | Ligament sprains, muscle strains, tendonitis | Clinic-based treatment |
| Interferential Therapy | Pain modulation & swelling reduction | Persistent or complex soft tissue/joint injuries | Mainly clinic-based |
Cultural Considerations in British Practice
It is important to note that the choice of electrotherapy in the UK is guided not only by clinical evidence but also by patient preference and accessibility within the NHS or private sectors. Physiotherapists here often engage patients in shared decision-making, fostering trust and promoting adherence to rehabilitation plans tailored to individual needs and lifestyles.
3. Clinical Applications for Specific Sports Injuries
In the UK, sports injuries such as sprains, strains, and overuse conditions are frequently encountered across all levels of physical activity, from community football pitches to elite athletic training grounds. Electrotherapy has become a mainstay in many rehabilitation programmes, offering tailored interventions that align with both best practice guidelines and patient-centred care. For instance, ultrasound therapy is often utilised to address soft tissue injuries like ankle sprains by promoting tissue repair and reducing swelling, which is particularly valuable during the acute phase of injury management.
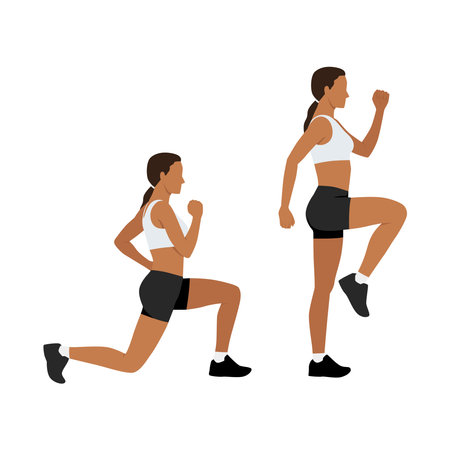
Strains—common among runners and those engaged in field sports—are frequently managed using modalities such as TENS (Transcutaneous Electrical Nerve Stimulation) or NMES (Neuromuscular Electrical Stimulation). These approaches help modulate pain and encourage gentle muscle activation, supporting early mobilisation without exacerbating discomfort. In cases of overuse injuries, such as tendinopathies seen in cricket bowlers or tennis players, clinicians may employ pulsed shortwave diathermy to enhance circulation and facilitate the healing process while minimising further tissue stress.
It is worth noting that electrotherapy protocols are always carefully adapted to the individual’s presentation and goals. British physiotherapists commonly integrate these techniques within broader rehabilitation strategies, combining hands-on manual therapy, graded exercise programmes, and education about injury prevention. This holistic approach not only reflects current evidence but also resonates with the UK’s ethos of providing compassionate, comprehensive care that supports athletes’ return to sport safely and confidently.
4. Guidelines and Regulations for Electrotherapy Practice in the UK
In the United Kingdom, the practice of electrotherapy within sports injury rehabilitation is governed by a combination of national regulations, professional standards, and evidence-based guidelines. These frameworks ensure that electrotherapy modalities are used safely, ethically, and effectively in clinical settings. Below is an outline of the main regulatory bodies and professional guidance relevant to practitioners in this field.
Key Regulatory Bodies
| Organisation | Role in Electrotherapy Regulation |
|---|---|
| Health and Care Professions Council (HCPC) | Regulates physiotherapists and sets standards for proficiency, conduct, and ethics. |
| Chartered Society of Physiotherapy (CSP) | Provides professional guidance, continuing education, and best practice resources. |
| National Institute for Health and Care Excellence (NICE) | Issues evidence-based recommendations regarding the use of medical technologies, including some electrotherapy applications. |
Professional Standards and Clinical Governance
Physiotherapists and sports clinicians must adhere to local trust or clinic protocols, as well as broader national guidelines. This ensures patient safety and upholds the profession’s reputation. Adherence includes:
- Maintaining up-to-date knowledge through CPD (Continuing Professional Development).
- Obtaining informed consent prior to treatment.
- Documenting assessments, interventions, and patient responses thoroughly.
- Ensuring equipment maintenance and safety checks as per manufacturer and legislative requirements (e.g., PUWER 1998).
NICE Guidelines on Electrotherapy Modalities
NICE regularly reviews the clinical efficacy of different electrotherapy techniques such as TENS, ultrasound therapy, and shockwave therapy. Recommendations may specify indications, contraindications, and levels of supporting evidence for each modality within musculoskeletal injury management.
Cultural Considerations in UK Sports Clinics
The UK places emphasis on patient-centred care—respecting individual preferences, values, and cultural backgrounds when planning treatment. Practitioners are encouraged to communicate clearly with patients about potential benefits and risks associated with electrotherapy. Additionally, documentation must meet GDPR standards for privacy and confidentiality.
Summary Table: Key Requirements for Safe Electrotherapy Practice
| Requirement | Description |
|---|---|
| Professional Registration | HCPC registration required for legal practice as a physiotherapist. |
| Evidence-Based Practice | Treatments should align with NICE or CSP guidance where available. |
| Patient Safety Checks | Regular equipment testing; adherence to safety protocols. |
| Record-Keeping & Consent | Comprehensive notes; clear patient communication & agreement. |
By following these guidelines and regulations, sports clinics across the UK can ensure high standards of care while minimising risk—fostering a supportive environment for athletes’ recovery journeys through the safe application of electrotherapy.
5. Integration into Multidisciplinary Rehabilitation Programmes
In the United Kingdom, sports injury rehabilitation is widely recognised as most effective when delivered through a multidisciplinary approach. Electrotherapy is seamlessly integrated alongside other therapeutic modalities, including physiotherapy, manual therapy, exercise prescription, and psychological support. This collaborative ethos is at the heart of British sports medicine, where practitioners work closely to design bespoke rehabilitation plans that address each athlete’s unique needs.
Electrotherapy’s role within these programmes is not isolated; rather, it complements traditional interventions by accelerating pain relief and tissue healing, thereby enabling earlier engagement in active rehabilitation strategies. For example, modalities such as TENS or ultrasound may be used initially to manage inflammation or discomfort, allowing athletes to participate more fully in physiotherapist-led exercises or strength training sessions.
This holistic and patient-centred approach aligns with NHS guidelines and professional standards across UK healthcare settings. Multidisciplinary teams—often comprising physiotherapists, sports physicians, occupational therapists, and sometimes psychologists—meet regularly to review progress and adapt interventions. The integration of electrotherapy within this framework fosters continuity of care and ensures that every aspect of the athlete’s physical and emotional wellbeing is considered throughout the recovery journey.
Ultimately, the thoughtful combination of electrotherapy with other therapies underscores the commitment to best practice in British sports medicine. By prioritising communication among professionals and involving patients in decision-making, rehabilitation becomes not just about treating injuries but also about empowering individuals to achieve optimal long-term outcomes.
6. Patient Perspectives and Practical Considerations
When considering the applications of electrotherapy in sports injury rehabilitation within the UK, it is essential to understand the patient perspective as well as the practicalities involved in accessing these treatments. Patients often approach electrotherapy with a sense of hope, seeking faster recovery and pain relief for their injuries. Many express positive experiences, particularly noting improvements in mobility and comfort following sessions. However, expectations can vary widely; some anticipate immediate results, while others appreciate gradual progress over time.
Accessing Electrotherapy through the NHS
In the UK, the National Health Service (NHS) provides a structured pathway for those requiring physiotherapy interventions, including electrotherapy. Typically, patients are referred by their GP or a specialist following an initial assessment. While NHS clinics do offer electrotherapy modalities such as ultrasound and TENS, availability can be limited due to high demand and resource constraints. As a result, waiting times may be longer, and not all patients will receive electrotherapy as part of their standard care package.
Private Clinics and Alternative Routes
For those seeking more immediate or tailored treatment, private physiotherapy clinics present an alternative. These settings often provide quicker access to a wider range of electrotherapy options, although this comes at a personal cost. Patients choosing private care generally report higher satisfaction with appointment flexibility and continuity of therapist support, yet affordability remains a concern for many.
Patient Expectations and Communication
A key factor in successful rehabilitation is clear communication between clinicians and patients regarding the goals and likely outcomes of electrotherapy. Managing expectations—whether through NHS or private care—is crucial. Patients benefit from understanding that electrotherapy is typically most effective when combined with exercise-based rehabilitation and other supportive therapies.
Ultimately, patient experiences with electrotherapy in the UK are shaped not only by clinical effectiveness but also by practical considerations such as accessibility, waiting times, and quality of interaction with healthcare professionals. Thoughtful guidance and empathetic support throughout the rehabilitation journey help ensure that individuals feel empowered and cared for during their recovery process.

