Overview of Arthritis in the UK
Arthritis is a significant health concern across the United Kingdom, affecting millions and impacting daily life for many. According to Versus Arthritis, over 10 million people in the UK are living with arthritis or other musculoskeletal conditions, making it one of the most prevalent chronic illnesses nationwide. The condition does not discriminate by age, though it is more commonly diagnosed among older adults—especially those over 45. However, younger individuals and even children can be affected, with around 15,000 children and young people under 25 living with arthritis in the UK. Among all types, osteoarthritis is the most frequently diagnosed form, particularly in weight-bearing joints like knees and hips. Rheumatoid arthritis is another common type, characterised by its autoimmune nature and tendency to impact women more often than men. Gout and psoriatic arthritis also contribute to the spectrum of arthritic conditions seen by healthcare professionals throughout England, Scotland, Wales, and Northern Ireland. These statistics highlight just how widespread and varied arthritis is within British society, affecting people from all walks of life and placing significant demand on NHS resources.
Arthritis and Musculoskeletal Health
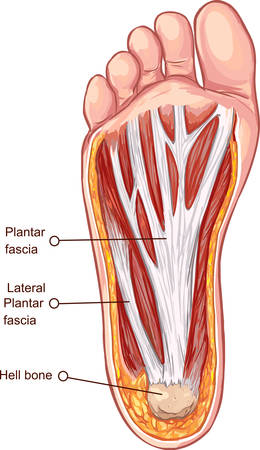
When we talk about arthritis in the UK, it’s crucial to understand its profound effects on musculoskeletal health. The musculoskeletal system is made up of bones, joints, muscles, ligaments, and tendons—all working together to support movement and daily function. Arthritis, particularly osteoarthritis and rheumatoid arthritis which are common across Britain, targets these structures in different but equally challenging ways.
How Arthritis Impacts Musculoskeletal Structures
At the core of arthritis is inflammation—a biological response that, while meant to protect, can result in pain and degeneration when chronic. Here’s a breakdown of how arthritis affects each part of the musculoskeletal system:
| Structure | Impact of Arthritis |
|---|---|
| Joints | Cartilage wears down, causing pain, stiffness, and reduced mobility. Swelling is common, making everyday activities like walking or gardening increasingly difficult. |
| Bones | As cartilage erodes, bones may rub against each other or develop growths (osteophytes). This can lead to deformity and persistent discomfort. |
| Muscles | Pain and limited joint movement often cause muscle weakness due to disuse. Over time, muscle mass may decrease around affected joints. |
| Ligaments | Chronic inflammation can weaken ligaments, resulting in instability and an increased risk of injury during routine activities. |
The Process of Degeneration and Inflammation
The cycle usually begins with minor symptoms—perhaps aching knees after a walk through Hyde Park or stiff fingers during cold British mornings. Over time, inflammation persists, leading to the breakdown of cartilage—the tissue that cushions joints. As cartilage thins out, bone surfaces become exposed and friction increases. The body tries to repair this damage but often creates excess bone (bone spurs) instead.
A Real-World Perspective from the UK
Living with arthritis isn’t just about physical pain; it’s about adapting your lifestyle. Many people across the UK find their hobbies—like hill walking in the Lake District or tending to an allotment—become more taxing. Understanding these musculoskeletal changes helps individuals seek timely advice from their GP or physiotherapist, making informed choices for managing symptoms and maintaining independence.
3. Daily Life Challenges for UK Patients
Living with arthritis in the UK brings a unique set of daily challenges that often go beyond physical discomfort. For many, the unpredictable nature of pain and stiffness means that even simple tasks—such as making a cuppa, getting dressed, or walking to the bus stop—can become daunting. British homes, with their traditional staircases and sometimes narrow hallways, can further complicate mobility. Workplaces are increasingly aware of these struggles, but not all employers fully understand the need for flexible working hours or ergonomic adjustments. The Equality Act 2010 offers some legal protection, yet patients often have to advocate persistently for reasonable adjustments like adapted chairs, voice recognition software, or phased return-to-work plans.
Public transport presents another hurdle. While London’s buses and trains are improving accessibility, rural areas may lack suitable facilities or support for those with limited mobility. Blue Badge parking schemes help, but finding available spaces remains a common frustration. Leisure activities—be it enjoying a walk along the seafront or joining a local gardening club—often require creative problem-solving. Many rely on community groups such as Versus Arthritis or local NHS pain management services for advice and support in adapting hobbies or social outings.
Despite these hurdles, people living with arthritis in the UK show remarkable resilience. They develop routines that balance activity with rest, learn to pace themselves, and make use of aids like kettle tippers or jar openers. Peer support—whether through online forums or local meet-ups—provides encouragement and practical tips specific to life in Britain. Ultimately, managing arthritis day-to-day is about accepting help when needed and embracing small victories, whether that’s getting out into the garden after a rainy spell or simply making it through a workday with less pain than before.
4. Impact on Mental Wellbeing
Living with arthritis in the UK extends far beyond physical symptoms; it takes a profound toll on mental wellbeing. The daily reality of managing persistent pain, reduced mobility, and uncertainty about the future can lead to a range of emotional and psychological challenges. Many people find themselves grappling with feelings of frustration, sadness, or even hopelessness as their independence is impacted and everyday activities become more difficult.
Isolation and Loneliness
Social isolation is a significant concern for those with arthritis. Limited mobility or chronic discomfort may make it challenging to participate in social events or maintain friendships. In the UK, where weather can often restrict outdoor activities and public transport may not always be accessible, these barriers can intensify feelings of loneliness. A lack of understanding from others can also make it harder for individuals to seek support or talk openly about their experiences.
The Psychological Burden of Pain Management
Persistent pain is mentally exhausting and can erode resilience over time. The unpredictability of flare-ups may lead to anxiety about making plans or attending work, further impacting confidence and self-esteem. British culture often values stoicism—just “getting on with it”—which might discourage people from expressing their struggles or seeking help for the emotional side of arthritis.
Access to Mental Health Support in the UK
The NHS does offer mental health services, but accessing specialist support tailored to chronic illness can be challenging due to long waiting times and regional disparities. Charities such as Versus Arthritis provide helpful resources and peer support networks, but there remains a need for greater integration between physical and mental healthcare services.
Mental Wellbeing Challenges Associated with Arthritis
| Challenge | UK Context Example | Potential Support Options |
|---|---|---|
| Isolation & Loneliness | Difficulty travelling to see friends due to limited public transport access in rural areas | Online peer support groups, community social prescribing schemes |
| Anxiety & Depression | Worrying about job security due to unpredictable sick days | NHS Talking Therapies, workplace adjustments, GP referrals |
| Lack of Understanding | Cultural reluctance to discuss mental health openly (“stiff upper lip”) | Awareness campaigns, support from charities like Mind or Versus Arthritis |
| Pain Management Stress | Struggling with medication side effects while awaiting specialist appointments | Pain management clinics, pharmacist consultations, patient education sessions |
Tackling Stigma and Building Resilience
Addressing the psychological impact of arthritis requires both personal strategies and systemic change. For many Brits living with arthritis, learning coping techniques—such as mindfulness, pacing activities, or reaching out for professional counselling—can be life-changing. At a societal level, more open conversations about invisible illnesses and investing in joined-up care are essential steps towards supporting mental wellbeing alongside musculoskeletal health.
5. Access to Healthcare and Support in the UK
Living with arthritis in the UK presents unique challenges, but there are robust support systems in place to help manage musculoskeletal health. The National Health Service (NHS) offers a clear pathway for diagnosis and ongoing care. Typically, patients first visit their GP, who can refer them to rheumatology specialists or physiotherapists for further assessment. Depending on the severity and type of arthritis, NHS treatment plans may include medication, physical therapy, pain management clinics, and occasionally surgical interventions such as joint replacement.
NHS Pathways for Arthritis Care
The NHS provides a multidisciplinary approach, combining medical treatment with practical advice on lifestyle changes. Patients often benefit from regular check-ups with specialist nurses and access to self-management courses designed to empower those living with arthritis. Waiting times can be variable depending on region, but initiatives like the NHS Long Term Plan have highlighted musculoskeletal conditions as a priority, aiming to improve early intervention and personalised care.
Local Charities and Community Support
Alongside medical care, local charities such as Versus Arthritis play a significant role in supporting individuals. These organisations offer helplines, peer support groups, educational workshops, and grants for mobility aids or home adaptations. Many communities across the UK have tailored services—like exercise classes or coffee mornings—specifically designed for people with arthritis, helping to reduce isolation and boost mental wellbeing.
Community Resources at Grassroots Level
Councils and local health authorities often collaborate with voluntary organisations to provide information hubs and drop-in centres where people can get advice on managing daily life with arthritis. Some regions also run pilot schemes offering digital tools or apps to track symptoms and facilitate direct communication between patients and healthcare professionals.
Recent Policy Initiatives
The UK government has recognised the growing impact of arthritis on public health. Recent policy developments focus on reducing waiting times for joint replacements, increasing funding for research into innovative treatments, and expanding social prescribing schemes that connect patients with non-medical support in their communities. These initiatives reflect a broader commitment to holistic care—addressing not only physical symptoms but also the emotional and social aspects of living with arthritis.
6. Personal Stories and Reflections
Living with arthritis in the UK is a journey that involves both physical and emotional adaptation. Many individuals across the country have found their own ways to manage daily life, demonstrating resilience and hope in the face of ongoing challenges. Take, for instance, Sarah from Manchester, who was diagnosed with rheumatoid arthritis in her early thirties. She recalls initially feeling overwhelmed but soon learned to pace herself, prioritise important activities, and embrace assistive devices without shame. Sarah’s experience highlights the importance of seeking support—be it from local arthritis groups or NHS resources—which helped her regain confidence and maintain her independence.
Adaptation in Everyday Life
For many UK residents, adapting to arthritis means making small yet significant changes at home and work. James, a retired teacher from Bristol, shares how he modified his kitchen to make cooking less strenuous, and how he uses voice-activated technology to keep in touch with friends and family. He points out that asking for help is not a sign of weakness but a practical step towards living well with arthritis.
The Power of Community
Support networks play a crucial role in fostering resilience. Groups such as Versus Arthritis offer both online forums and local meet-ups where people can share experiences and coping strategies. Claire from Edinburgh says these connections have been invaluable: “Knowing others understand what you’re going through makes all the difference—it’s about sharing tips, but also having a laugh together when days are tough.”
Looking Forward With Hope
While arthritis poses undeniable challenges, these personal stories underscore a common thread of hope. Advances in treatment, greater awareness around musculoskeletal health, and improved workplace accommodations mean that more people in the UK are able to live fulfilling lives despite their diagnosis. As one participant put it, “Arthritis may change your life, but it doesn’t define it. There’s always room for new goals, new hobbies, and new joys.”