Overview of Shoulder Injuries in the UK
Shoulder injuries are a significant concern across the UK, affecting people from all walks of life. These injuries are not confined to athletes or those with physically demanding jobs; they also frequently impact individuals due to age-related changes and everyday activities. In British society, shoulder problems often arise from three main sources: sports participation, occupational hazards, and the natural ageing process. Sports such as rugby, cricket, football, and tennis are popular throughout the country and commonly contribute to acute injuries like dislocations, rotator cuff tears, and labral damage. On the work front, jobs that involve repetitive overhead movements—such as construction, painting, or warehouse roles—can lead to overuse syndromes and chronic pain. Meanwhile, as the population ages, degenerative conditions like osteoarthritis and tendinopathy become more prevalent among older adults. Understanding these patterns is essential for both preventing injury and designing effective rehabilitation strategies tailored to the unique needs of people living in the UK.
Identifying Common Shoulder Injuries
When it comes to shoulder pain in the UK, several injuries tend to crop up more frequently than others. Whether you’re an office worker from Manchester, a tradesperson in Birmingham, or a keen tennis player in London’s parks, understanding these conditions can help spot issues early and guide your next steps towards recovery. Let’s take a closer look at the most common shoulder injuries seen across Britain.
Rotator Cuff Tears
The rotator cuff is a group of muscles and tendons that keep your shoulder stable and allow for smooth movement. Tears in this area are widespread—especially among people over 40 or those who do repetitive overhead work, such as painters or builders. Typical symptoms include shoulder weakness, difficulty lifting the arm, and aching pain that often disturbs sleep. In the British context, many cases arise from gradual wear-and-tear rather than sudden trauma, particularly due to our ageing population and prevalence of manual labour roles.
Frozen Shoulder (Adhesive Capsulitis)
This condition is characterised by stiffness and persistent pain, making everyday activities like putting on a jumper a real challenge. Frozen shoulder often affects people aged 40-60 and is more common if you’ve had recent shoulder surgery or immobilisation after an injury—a scenario familiar to many following falls on icy pavements during British winters. The hallmark symptom is restricted range of motion, both actively and passively.
Dislocations
Shoulder dislocations occur when the upper arm bone pops out of the socket. While this may sound dramatic, it’s relatively common in contact sports such as rugby or hockey—both popular across the UK—or after slips and trips, especially among older adults. Symptoms include intense pain, visible deformity, and inability to move the joint. Recurrence is also a concern, particularly for younger individuals involved in high-impact sports.
Tendinitis
Tendinitis refers to inflammation of the shoulder tendons, usually resulting from repetitive strain or overuse. It’s not just athletes who are affected; gardeners spending hours pruning roses or office workers with poor desk setups are equally at risk. Classic signs include aching pain that worsens with activity and tenderness around the joint.
Comparison Table: Key Features of Common Shoulder Injuries in the UK
| Condition | Main Symptoms | Common Causes (UK Context) |
|---|---|---|
| Rotator Cuff Tear | Weakness, night pain, limited lift | Ageing workforce, manual jobs, falls |
| Frozen Shoulder | Stiffness, severe pain, limited movement | Post-injury immobilisation, cold weather accidents |
| Dislocation | Shooting pain, deformity, immobility | Contact sports (rugby), falls on ice/slippery surfaces |
| Tendinitis | Dull ache, activity-related pain, tenderness | Repetitive tasks (gardening), poor ergonomics at work |
A Practical Note for British Readers
If you notice persistent discomfort or loss of function after a fall on wet cobbles or following a weekend of DIY gone wrong, don’t ignore it. Early identification means quicker access to effective rehabilitation—something our NHS physios across the country excel at when problems are caught promptly.
3. Diagnosis and NHS Pathways
When it comes to shoulder injuries in the UK, understanding the diagnostic process and how the National Health Service (NHS) operates is essential for both patients and practitioners. Most people in Britain will first consult their GP (General Practitioner) when experiencing persistent shoulder pain or a sudden injury. GPs are well-versed in identifying common shoulder issues, such as rotator cuff tears, frozen shoulder, or impingement syndrome, but they often rely on a combination of clinical assessment and patient history as a starting point.
After an initial examination, your GP may recommend conservative management—such as rest, over-the-counter pain relief, or physiotherapy referral—as a first step. If symptoms persist or if there are signs of more complex damage, you might be referred for imaging, most commonly an X-ray or ultrasound via the NHS. In some cases where diagnosis remains unclear or surgical intervention is considered, an MRI scan could be arranged, though waiting times can vary significantly across different NHS trusts.
The pathway through the NHS can sometimes feel like a bit of a maze, especially with pressure on resources and waiting lists. However, the system is designed to ensure that those with urgent needs are prioritised. For many patients, seeing an NHS physiotherapist is a key stage; these professionals play a vital role in both assessment and ongoing rehabilitation planning. They’ll work with you to create an individualised rehab protocol tailored to your specific injury and lifestyle demands—a crucial step towards recovery that reflects best practice across the UK.
For those who need specialist input—for example from an orthopaedic consultant—the referral process continues within the NHS framework. While this can require patience due to appointment backlogs, it’s important to stay proactive: keep your GP updated on your progress and don’t hesitate to ask about alternative options such as community MSK (musculoskeletal) clinics if your area offers them. From my experience working alongside NHS teams, being informed and engaged really helps you make the most of what’s available—ultimately leading to better outcomes for your shoulder health.
4. Effective Rehabilitation Protocols
In the UK, evidence-based rehabilitation for shoulder injuries is paramount to restoring function and preventing recurrence. Clinical guidelines advocate a multidisciplinary approach, with physiotherapy at its core. British physiotherapists commonly employ a combination of manual therapy, tailored exercise programmes, and patient education, all grounded in current research and NHS best practices.
Physiotherapy Approaches in the UK
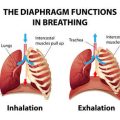
Initial management often includes pain control and inflammation reduction through modalities like ice packs or prescribed analgesics by GPs. Early mobilisation is encouraged to avoid stiffness, particularly for frozen shoulder or post-operative recovery. Manual therapy techniques such as joint mobilisations and soft tissue massage are widely used to enhance range of motion and reduce discomfort.
Progressive Exercise Protocols
Rehabilitation exercises are typically introduced in stages, respecting tissue healing timelines and individual capability. The following table outlines a sample progression recommended in UK clinics:
| Phase | Focus | Example Exercises |
|---|---|---|
| Acute (0-2 weeks) | Pain relief & gentle mobility | Pendulum swings, passive assisted elevation |
| Subacute (2-6 weeks) | Restore range & activate muscles | Wall crawls, isometric holds |
| Strengthening (6+ weeks) | Build stability & endurance | Theraband external rotations, scapular retractions |
Patient Education and Self-management
A key aspect of successful rehab in the UK is empowering patients with knowledge about their injury, expected recovery timelines, and warning signs that warrant further assessment. NHS clinicians often provide written leaflets or digital resources so individuals can safely continue exercises at home—a practice that enhances long-term outcomes and aligns with the self-care ethos prevalent in British healthcare culture.
Collaborative Goal Setting
Lastly, rehabilitation is most effective when goals are set collaboratively between patient and therapist. This fosters motivation and accountability, ensuring protocols are personalised to each person’s work demands, hobbies, and lifestyle—a hallmark of quality care within the UK system.
5. Everyday Tips and Self-Management
Managing shoulder injuries at home can be both practical and effective, especially when you tailor your approach to fit the typical British lifestyle. Below are some tried-and-tested strategies, gathered from both clinical practice and everyday experience, to help you maintain progress between professional appointments and minimise disruption to daily life.
Making Daily Activities Shoulder-Friendly
If you live in a typical UK household—perhaps an older property with stairs or a narrow kitchen—you’ll need to adapt certain routines. For example, when reaching for items on high shelves, use a step stool rather than overstretching. Carry shopping bags close to your body and split heavy loads into smaller, manageable portions. For those commuting by train or bus, try to avoid hanging from overhead rails; instead, hold onto vertical poles at waist height.
Establishing a Home Exercise Routine
Consistency is key in rehabilitation. Set aside five to ten minutes twice a day for prescribed exercises such as pendulum swings or gentle range-of-motion movements. You don’t need fancy equipment—a tin of beans works well as a light weight for strengthening. Place sticky notes in visible spots (like the kettle or bathroom mirror) as reminders. If you find motivation slipping, enlist a friend or family member for accountability—a very British approach is to “keep calm and carry on” together.
Pacing Yourself and Managing Pain
It’s tempting to push through pain, but pacing is crucial for healing. Alternate activity with rest: after gardening or DIY, give your shoulder a break with a cuppa and gentle stretching. Use ice packs wrapped in a tea towel for 10-15 minutes after activity if your shoulder feels sore (avoid direct contact with skin). Over-the-counter pain relief like paracetamol or ibuprofen can be helpful, but always follow NHS guidelines or consult your pharmacist first.
Knowing When to Seek Professional Help
While self-management is valuable, some signs mean it’s time to book an appointment with your GP or physiotherapist. If you notice worsening pain that doesn’t improve with rest, significant swelling, numbness, tingling, or loss of strength, don’t wait it out—get checked promptly. The NHS 111 service is a reliable point of contact for advice if you’re unsure. Early intervention can make all the difference in preventing long-term issues.
In Summary
Combining practical home adaptations, regular gentle exercise, sensible pacing, and knowing when to seek help forms the backbone of effective shoulder injury management in the UK. With these strategies rooted in everyday British life—and a bit of perseverance—you’ll give yourself the best chance of recovery while maintaining your independence and routine.
6. Personal Stories: Navigating Recovery in the UK
Shoulder injuries can be deeply personal experiences, affecting every aspect of daily life and wellbeing. Across the UK, countless individuals have faced the daunting path of recovery, each journey marked by unique challenges and moments of triumph. In this section, we delve into some heartfelt reflections and real-life accounts that shed light on what it truly means to recover from common shoulder injuries within the British healthcare context.
Facing the Initial Setback
For many patients, like Sarah from Manchester, the shock of a rotator cuff tear brought an abrupt halt to her active lifestyle. “The pain was overwhelming at first,” she recalls, “and I worried about losing my independence.” After her diagnosis through the NHS, Sarah felt both relief at having clarity and anxiety about what lay ahead. Her GP’s reassurance and clear explanation of the rehabilitation process helped ease her concerns, highlighting the importance of communication in patient care.
The Role of Community and Support
In London, Tom—an avid cyclist—found his dislocated shoulder not only physically limiting but also mentally taxing. “I underestimated how much my mood would be affected,” he admits. What made a difference for Tom was joining a local support group run by his physiotherapy clinic. Sharing stories with others navigating similar struggles fostered a sense of camaraderie and hope. “It wasn’t just about exercises; it was about feeling understood,” Tom reflects.
Challenges Along the Way
Even with access to rehabilitation protocols, setbacks are common. Lisa, a nurse in Birmingham, faced repeated flare-ups during her recovery from frozen shoulder. “There were days when progress seemed to stall completely,” she says. However, regular check-ins with her NHS physiotherapist kept her motivated. Lisa emphasises the importance of patience: “In the UK system, sometimes waiting lists can be long, but persistence pays off.”
Celebrating Successes—Big and Small
Despite these hurdles, many patients celebrate milestones that might seem minor to others—raising an arm above shoulder height or sleeping through the night without pain. For Mark in Edinburgh, returning to gentle hill walks after months of rehab felt like regaining a piece of himself. Practitioners echo this sentiment: “Every bit of progress counts,” says Emma, a senior physio in Leeds. “We encourage our patients to acknowledge their achievements as they come.”
Ultimately, these personal stories underscore that shoulder injury recovery is rarely linear—but with support from practitioners, community resources, and a resilient mindset, meaningful improvement is possible. These lived experiences not only offer hope to those currently on their own recovery journeys but also highlight the value of compassionate care within the UK’s unique healthcare landscape.