Introduction to Shoulder Injuries in UK Rugby
Rugby is deeply woven into the fabric of British sporting culture, celebrated for its physicality, camaraderie, and intensity. However, this intensity comes at a cost—shoulder injuries are among the most common complaints faced by rugby players across all levels in the UK. From local club matches on muddy pitches to elite Premiership clashes, shoulder issues can sideline even the toughest athletes. The most frequently encountered injuries include rotator cuff tears, acromioclavicular (AC) joint sprains, dislocations, and labral tears. These injuries are often the result of high-impact tackles, falls, and scrums where forceful contact is unavoidable.
The impact of shoulder injuries extends far beyond individual pain and recovery time. For players, these injuries can dramatically affect their ability to pass, tackle, and maintain form—key elements of rugby performance. On a broader level, when a key player is out due to a shoulder injury, team dynamics inevitably shift. Coaches may need to reshuffle line-ups or change tactics mid-season, affecting both morale and results. This makes effective physiotherapy not just a matter of personal health but a critical component in maintaining team cohesion and competitive edge throughout the rigorous rugby season.
2. Assessment and Early Intervention
When it comes to managing shoulder injuries in UK rugby players, swift and accurate assessment is absolutely vital. Rugby’s fast pace and physical intensity mean that even minor shoulder issues can quickly escalate if not addressed immediately. As physiotherapists working with rugby teams across the country, we rely on a combination of hands-on experience and evidence-based techniques to ensure our players get back on the pitch safely and efficiently.
Key Physiotherapy Assessment Methods
The initial assessment typically begins pitchside, where a structured approach is essential. The following table outlines the primary assessment methods used:
| Assessment Method | Purpose | Relevance to Rugby |
|---|---|---|
| Observation & History Taking | Identify mechanism of injury and visible deformities | Crucial for distinguishing between traumatic and overuse injuries in contact situations |
| Palpation | Detect swelling, tenderness, or abnormal movement | Helps pinpoint specific structures affected after tackles or falls |
| Range of Motion (ROM) Tests | Assess active and passive movement limitations | Quickly reveals functional impairments relevant to gameplay |
| Special Tests (e.g., Apprehension Test, Hawkins-Kennedy) | Diagnose instability or impingement syndromes | Commonly used due to high incidence of dislocations and impingements in rugby |
| Strength Testing | Evaluate muscle power around the shoulder girdle | Essential for identifying weaknesses that may compromise performance or increase re-injury risk |
Immediate Care Strategies Post-Injury
After the initial assessment, early intervention is key. The following strategies are standard practice among UK rugby physios:
- P.R.I.C.E Protocol (Protection, Rest, Ice, Compression, Elevation): Applied immediately to reduce inflammation and prevent further damage.
- Pain Management: Use of appropriate analgesia or taping methods to support the joint and limit discomfort during acute phases.
- Immobilisation: For suspected dislocations or fractures, immobilising the arm in a sling until further imaging can be arranged—often crucial given the remote locations of some British rugby pitches.
- Communication: Clear reporting to coaches, medical staff, and when necessary, referring on for further investigation (such as X-ray or MRI) at NHS or private clinics.
The Importance of Timeliness in Rugby Contexts
The contact-heavy nature of rugby means that delays in addressing shoulder injuries can have long-term consequences—not just for individual players but also for team dynamics. Early recognition and intervention help minimise time away from training and matches, supporting both player welfare and squad performance. From my own experience on chilly Saturday afternoons in the North East leagues to the high-stakes environments of university championships, a rapid yet thorough approach has consistently proven itself invaluable.
3. Manual Therapy Approaches
For rugby players in the UK, manual therapy remains a cornerstone of physiotherapy intervention when managing shoulder injuries. Rugby’s physical demands mean that players often sustain issues such as rotator cuff strains, AC joint sprains, and general shoulder instability. Physiotherapists across the UK utilise a range of hands-on techniques specifically tailored to the needs of rugby athletes, focusing not just on recovery but also on enhancing performance and preventing re-injury.
Joint Mobilisations
One of the most popular manual therapy methods in British physiotherapy practice is joint mobilisation. This technique involves skilled, passive movements applied to the shoulder joint to improve mobility, reduce pain, and restore normal function. For rugby players, Grade I and II mobilisations are commonly used in the acute phase to decrease pain and muscle guarding, while more advanced grades may be incorporated as healing progresses. Mobilisations are often adapted depending on whether the athlete is a forward or back, given their different playing roles and injury profiles.
Soft Tissue Work
Hands-on soft tissue techniques are another mainstay in treating rugby-related shoulder injuries. Methods such as deep tissue massage, trigger point release, and myofascial release aim to reduce muscle tension, break down adhesions, and promote circulation in overused or traumatised muscles like the deltoids, rotator cuff group, and upper trapezius. UK physios often combine soft tissue work with active rehabilitation exercises to maximise flexibility and function – crucial for players returning to full-contact training.
Taping Techniques
Taping is widely recognised across British rugby clubs for its role in both injury management and prevention. Kinesiology taping and rigid sports tape are frequently used by physios to provide proprioceptive feedback, reduce pain, support unstable joints, or offload stressed tissues during matches and training sessions. Techniques are carefully individualised: for example, taping the AC joint after a sprain or supporting the scapula for those with instability issues. Many UK clubs even train their athletes in basic taping methods so they can maintain support between physio sessions.
Bringing It All Together
The effectiveness of manual therapy for shoulder injuries in UK rugby lies in its adaptability and evidence-based application. British physios blend these hands-on techniques with ongoing clinical assessment and communication with coaching staff to ensure that each player receives bespoke care. This practical approach not only accelerates recovery but also empowers athletes to take an active role in their rehabilitation journey – something that resonates deeply within the UK rugby culture.
4. Exercise Rehabilitation and Strengthening
Rehabilitation exercise routines play a pivotal role in the recovery of shoulder injuries among UK rugby players. Physiotherapists across the UK often employ a combination of evidence-based exercises tailored to the unique demands of rugby, focusing on restoring both strength and stability to the injured shoulder. Below, I’ll walk you through some core techniques and how they are typically implemented in a structured rehabilitation programme.
Progressive Exercise Protocols
The rehabilitation journey usually begins with gentle range-of-motion (ROM) exercises and progresses toward advanced strengthening drills. This staged approach not only prevents re-injury but also aligns with the practical realities of returning to a contact-heavy sport like rugby. A typical progression might look like this:
| Phase | Key Exercises | Goals |
|---|---|---|
| Early Stage | Pendulum swings, assisted ROM, isometric holds | Reduce pain, restore basic mobility, prevent stiffness |
| Mid Stage | Theraband external/internal rotations, scapular setting, wall slides | Begin muscle activation, improve proprioception, maintain flexibility |
| Late Stage | Resistance band work, dumbbell raises, press-ups plus, plyometrics | Build strength, enhance dynamic stability, prepare for sport-specific movement |
Emphasis on Functional Stability
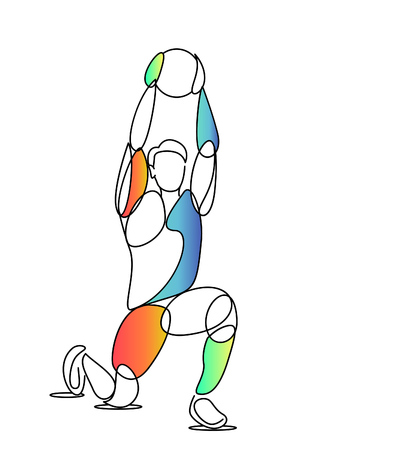
UK physiotherapists pay particular attention to functional stability by integrating closed kinetic chain exercises and proprioceptive training into their routines. For instance, exercises such as ‘plank-to-press’ transitions or medicine ball throws are commonly used to mimic the unpredictable demands of rugby while enhancing neuromuscular control.
Common UK Physiotherapy Techniques:
- Scapular Retraining: Essential for ensuring proper shoulder mechanics during tackling or line-out lifts.
- Cuff Strengthening: Targeting rotator cuff muscles through resistance bands to support joint integrity under load.
- Plyometric Drills: Medicine ball slams and rebound catches to simulate match scenarios and promote explosive power.
- Sport-Specific Integration: Gradual reintroduction to contact drills under supervision once foundational strength is restored.
The Importance of Individualisation
No two shoulder injuries—or players—are alike. UK physiotherapists draw upon their clinical experience to adapt protocols based on factors like player position, previous injury history, and season timing. This personalised approach maximises outcomes while minimising risk.
5. Injury Prevention and On-Field Management
When it comes to rugby in the UK, injury prevention is just as crucial as effective rehabilitation. Physiotherapists working with rugby teams are keenly aware that preventing re-injury is the foundation for long-term athletic performance and player safety. In British rugby culture, prevention strategies are deeply embedded into both training routines and match-day protocols.
Warm-Up Drills: The First Line of Defence
A robust warm-up is non-negotiable on any rugby pitch across the UK. Physiotherapists advocate for dynamic stretching and activation drills tailored to shoulder mobility and stability. Arm swings, resistance band exercises, and controlled contact simulations not only prepare the muscles for impact but also reinforce neuromuscular patterns that protect the shoulder joint during tackles and scrums.
Movement Screening: Spotting Risks Early
British physiotherapists often implement pre-season and mid-season movement screening sessions. These screenings help identify players at higher risk of shoulder injuries due to imbalances or previous trauma. Functional movement assessments—such as overhead reach, scapular control tests, and rotator cuff strength evaluations—allow physiotherapists to personalise prehabilitation programmes and address weaknesses before they become problematic.
Advice for Coaches: Creating a Culture of Prevention
For coaches, fostering a team culture that values injury prevention is key. Encouraging adherence to physiotherapist-recommended warm-up routines, ensuring adequate rest between high-contact drills, and promoting open communication about niggles or discomfort can make a significant difference. Coaches should also be proactive in rotating players during matches and training to avoid overuse injuries, especially among younger athletes who may be more susceptible.
Player Responsibility: Taking Ownership of Recovery
Players themselves play a vital role in prevention by committing to prescribed home exercise programmes, maintaining good technique in tackles, and reporting any signs of discomfort early. Education around self-management—such as icing after matches, recognising red flags for injury recurrence, and following return-to-play protocols—is a hallmark of best practice in British rugby physiotherapy circles.
Ultimately, integrating these evidence-based strategies into daily routines ensures that both coaches and players are well-equipped to manage shoulder health proactively, keeping everyone on the pitch longer and performing at their best throughout the gruelling UK rugby season.
6. Return-to-Play Protocols and Psychological Support
When it comes to returning UK rugby players to the pitch after a shoulder injury, physiotherapists follow a meticulously structured protocol that balances physical readiness with psychological resilience. This approach is deeply rooted in both clinical best practice and the unique demands of British rugby culture, where player welfare is paramount but so too is the drive for competitive excellence.
Physical Criteria: Gradual Progression and Objective Measures
The return-to-play process begins only once all physical criteria are objectively met. This includes full, pain-free range of motion in the shoulder, restoration of muscle strength (often benchmarked against the uninjured side), and successful completion of functional rugby-specific drills. UK physios use validated assessment tools such as the Oxford Shoulder Score and employ gradual loading protocols—starting with non-contact training, progressing to controlled contact, and finally integrating the player into full match situations. Clear communication between medical staff, coaches, and players ensures each step is tailored to individual recovery while minimising re-injury risk.
Stage-Based Return: From Clinic to Club
Most clubs in the UK follow a phased system: initial rehab at the clinic, then pitch-based conditioning, then team integration. At every stage, physios continually reassess not just the shoulder’s biomechanics but also overall movement quality under fatigue—mirroring real match conditions. Players must demonstrate confidence in tackling, passing, and scrummaging before being cleared for competitive play.
Mental Resilience: Supporting the Player’s Mindset
Physical readiness is just one piece of the puzzle; psychological support is equally critical in British rugby’s high-pressure environment. Many physiotherapists collaborate with sports psychologists or offer their own mental skills coaching. This might include addressing fear of re-injury, managing performance anxiety, and rebuilding self-belief through visualisation techniques or graded exposure to challenging drills. Peer support within the team plays a huge role—UK rugby culture values camaraderie and mutual encouragement, helping injured players reintegrate socially as well as physically.
Holistic Communication: Keeping Everyone in the Loop
A hallmark of effective UK physiotherapy practice is open dialogue—not just with athletes, but also coaches, strength & conditioning staff, and families. Regular check-ins help identify any lingering doubts or barriers to return. By blending evidence-based protocols with genuine empathy for each player’s journey, physios ensure that when a rugby player steps back onto the pitch, they’re truly ready—in body and mind—to embrace the challenge ahead.


