Introduction to Spinal Cord Injury Rehabilitation in the UK
Spinal cord injury (SCI) rehabilitation in the United Kingdom is a multifaceted and evolving field, driven by a commitment to delivering holistic, patient-centred care. Across England, Scotland, Wales, and Northern Ireland, specialist NHS spinal injury centres and community-based services work collaboratively to support individuals and their families throughout their rehabilitation journey. The landscape of SCI rehabilitation reflects the UK’s dedication to inclusivity, dignity, and empowerment—values embedded within the NHS constitution. This approach not only addresses the physical aspects of recovery but also considers psychological wellbeing, social integration, and long-term independence. The combination of multidisciplinary expertise, evidence-based interventions, and person-focused support underpins current best practices in the UK, ensuring that every individual has access to compassionate care tailored to their unique needs.
2. Initial Assessment and Multidisciplinary Team Involvement
In the United Kingdom, the journey of spinal cord injury (SCI) rehabilitation begins with a robust initial assessment, ensuring that every individual’s needs are understood in their entirety. Early assessment protocols are not only clinical but are also deeply person-centred, reflecting the holistic ethos of UK healthcare. Upon admission to a specialist spinal unit or rehabilitation centre, patients undergo thorough physical, psychological, and social evaluations. These assessments are guided by NICE guidelines and national standards to establish a foundation for bespoke care planning.
The Role of the Multidisciplinary Team (MDT)
Central to the UK approach is the involvement of a multidisciplinary team (MDT), whose collaborative input shapes comprehensive rehabilitation strategies. The MDT typically includes consultants in spinal injuries, specialist nurses, physiotherapists, occupational therapists, psychologists, speech and language therapists where appropriate, social workers, and dietitians. Each professional brings unique expertise to the table:
| Professional | Primary Responsibilities |
|---|---|
| Consultant (Spinal Injuries) | Leads medical management, oversees diagnosis, and coordinates complex care needs. |
| Nurse Specialist | Provides ongoing clinical care, wound management, education on self-care, and emotional support. |
| Physiotherapist | Assesses mobility and function; develops individualised movement and strengthening programmes. |
| Occupational Therapist | Evaluates daily living skills; suggests adaptive equipment and home modifications. |
| Psychologist | Supports emotional adjustment; addresses mental health and coping strategies. |
| Social Worker | Liaises with community resources; assists with discharge planning and benefits advice. |
| Dietitian | Advises on nutritional needs to promote healing and prevent complications. |
Bespoke Care Planning: An Ongoing Conversation
The initial assessment is not a one-off event but marks the beginning of an ongoing dialogue between the patient, their family or carers, and the MDT. Together, they develop a tailored care plan that sets short- and long-term goals—focusing on maximising independence while respecting personal preferences and cultural values. This collaborative approach underpins best practice in UK SCI rehabilitation and ensures every individual’s journey is treated with dignity, compassion, and hope.
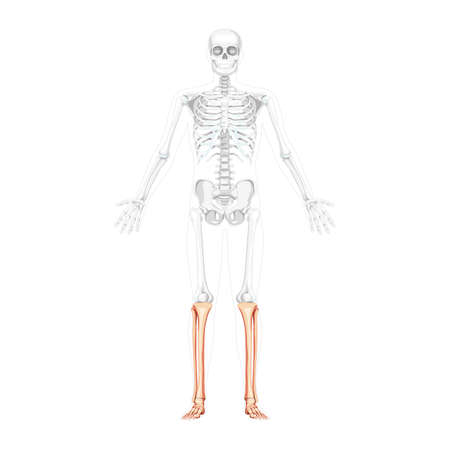
3. Physical Rehabilitation and Mobility Support
In the UK, physical rehabilitation for individuals with spinal cord injuries is a highly collaborative and person-centred process. Physiotherapy remains a cornerstone of rehabilitation, focusing not only on muscle strength and flexibility but also on managing spasticity, enhancing cardiovascular fitness, and preventing secondary complications such as pressure sores. British physiotherapists work closely with patients to develop tailored exercise regimes, mindful of each individual’s goals and lifestyle—whether that means returning to work, engaging in community activities, or simply regaining independence in personal care.
Physiotherapy: Maximising Movement and Function
Best practice in physiotherapy emphasises early intervention and consistent review throughout the rehabilitation journey. In many NHS trusts, multidisciplinary teams meet regularly to adapt plans as patients progress, ensuring that therapy remains responsive to changing needs. Hydrotherapy pools, gym-based sessions, and even outdoor mobility training in local parks are frequently used to mirror real-life situations encountered across the UK’s varied environments.
Occupational Therapy: Enabling Everyday Independence
Occupational therapists play a vital role in bridging hospital-based rehabilitation with everyday British life. They assess home environments, suggest practical adaptations (such as stairlifts or adapted bathrooms), and support re-engagement in meaningful daily activities. A key aspect is personalised goal-setting—helping individuals resume cooking a Sunday roast, gardening in an allotment, or simply accessing local shops independently. Occupational therapists also provide training on energy conservation techniques and safe transfer methods to maximise autonomy within the home and community.
Assistive Technology: Empowering Mobility Choices
The integration of assistive technology is increasingly central to best practice in spinal cord injury rehabilitation across the UK. From lightweight manual wheelchairs suited for navigating cobbled city centres, to advanced powered chairs designed for rural terrain, selection is based on lifestyle needs and personal preferences. Adapted vehicles with hand controls or wheelchair lifts can open up travel opportunities beyond public transport routes—an important consideration given the UK’s diverse geography. Additionally, emerging smart home technologies are enabling greater control over living environments through voice commands or adaptive switches.
Holistic Support for Life in the Community
The ultimate goal of physical rehabilitation and mobility support is to empower each individual to participate fully in British society. Services are designed not just to restore function but to foster confidence and social inclusion—from accessible sports clubs supported by organisations like WheelPower to peer mentoring schemes that connect newly injured people with those who have navigated similar journeys. Through these comprehensive approaches, individuals are supported with both practical tools and compassionate guidance as they rebuild their lives within the vibrant fabric of UK communities.
4. Psychological and Emotional Wellbeing
Addressing psychological and emotional wellbeing is a vital component of spinal cord injury rehabilitation in the UK. Beyond physical recovery, individuals often face profound life changes that can impact their mental health. Recognising this, current best practices place a strong emphasis on providing holistic support that nurtures both mind and spirit. The journey can feel overwhelming at times, but kindness, patience, and companionship are essential in fostering resilience and hope.
Mental Health Support: A Cornerstone of Care
Specialist rehabilitation centres across the UK integrate psychological care into their programmes. Access to qualified clinical psychologists, counsellors, and psychotherapists is standard practice, ensuring tailored support for patients as they process trauma, adjust to new circumstances, and manage ongoing emotional challenges. The NHS offers both inpatient and outpatient mental health services, while charities like the Spinal Injuries Association (SIA) provide additional resources specific to spinal cord injuries.
Peer Mentoring: Learning from Shared Experience
Peer mentoring plays an invaluable role in supporting those with spinal cord injuries. Connecting with someone who has navigated similar experiences can offer practical advice, encouragement, and a sense of belonging. Many UK-based organisations facilitate peer mentoring schemes:
| Organisation | Description | Contact/Resource |
|---|---|---|
| Spinal Injuries Association (SIA) | Peer support officers with lived experience offer one-to-one guidance. | SIA Peer Support |
| Back Up Trust | Mentoring services for all ages; group activities to build confidence. | Back Up Mentoring |
| Aspire | Community events and peer groups focused on independent living. | Aspire UK |
Family Counselling: Strengthening Relationships
The ripple effect of a spinal cord injury touches the whole family. Family counselling is offered by most major rehabilitation centres in the UK and supported by community mental health teams. These sessions help families adapt together, improve communication, and develop coping strategies in a safe environment. Charities such as Headway and Relate also extend family-specific services tailored to neurological injuries and long-term care needs.
Community Groups: Building Resilience Together
Across the UK, local community groups provide safe spaces for individuals and families affected by spinal cord injury to connect, share experiences, and nurture friendships. These groups foster resilience through acts of kindness—whether it’s sharing a cup of tea at a local meet-up or supporting each other online. The importance of these networks cannot be overstated; they remind everyone involved that they are not alone on their journey towards recovery and adaptation.
5. Community Reintegration and Social Inclusion
Strategies for Community Reintegration
Rejoining the community after a spinal cord injury (SCI) is both an important milestone and a complex process for individuals in the UK. Rehabilitation teams work closely with patients to develop tailored plans that support gradual reintroduction into daily life, taking into account physical capabilities, emotional well-being, and personal aspirations. This holistic approach often includes home assessments, family education, and peer mentoring schemes. Collaborative goal setting empowers individuals to regain independence at their own pace, supported by regular follow-ups from NHS community rehabilitation services.
Accessibility within UK Infrastructure
Improving accessibility is central to fostering inclusion across towns and cities in the UK. The Equality Act 2010 mandates reasonable adjustments to public spaces, transport, and housing. Local councils frequently partner with organisations such as AccessAble to provide up-to-date information about accessible routes, venues, and facilities. Despite ongoing progress, challenges remain—particularly in historic areas—yet continued advocacy from groups like Spinal Injuries Association drives further improvements in infrastructure and public awareness.
Vocational Rehabilitation
Returning to meaningful employment is a priority for many people following SCI. Vocational rehabilitation services in the UK offer practical support with CV writing, interview preparation, workplace adaptations, and liaison with employers under the Access to Work scheme. Occupational therapists work alongside job coaches to help individuals explore new career paths or adapt existing roles. There is also growing recognition of remote working opportunities, which can further facilitate participation in the workforce.
Opportunities for Social Engagement
Social connection is a vital aspect of long-term well-being after SCI. Across the UK, local and national support networks offer a range of social activities—from adaptive sports clubs to arts workshops and peer-led coffee mornings. Organisations like Back Up Trust and Aspire provide platforms for sharing experiences, building friendships, and accessing practical advice. Online communities have become increasingly important for those living in rural areas or seeking flexible ways to connect with others facing similar challenges.
A Gentle Pathway Forward
Community reintegration and social inclusion are ongoing journeys rather than single events. By drawing on a comprehensive mix of medical expertise, policy support, accessible infrastructure, and compassionate peer networks, individuals with spinal cord injury in the UK are gently empowered to reclaim active roles within their communities—supported every step of the way.
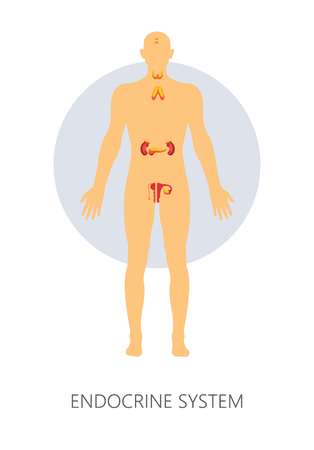
6. Long-term Management and Ongoing Support
Long-term management is a crucial element in the journey of individuals living with spinal cord injuries (SCI) in the UK. Beyond the initial rehabilitation phase, ongoing medical follow-up ensures that any evolving needs or potential complications are identified and addressed promptly. Regular reviews with multidisciplinary teams—often coordinated through NHS spinal injury centres—help monitor neurological status, bladder and bowel function, skin integrity, and mental health. Preventing secondary complications such as pressure ulcers, urinary tract infections, spasticity, and osteoporosis remains a priority throughout life. Education for individuals and their families on self-care and early warning signs is consistently reinforced to support independence and well-being.
The Importance of Community-Based Services
Community-based long-term care services play an invaluable role in sustaining quality of life. Occupational therapists, district nurses, physiotherapists, and social workers collaborate to deliver person-centred care plans tailored to changing needs. Access to home adaptations, mobility aids, and personal assistance can be facilitated through local authorities or NHS continuing healthcare. The emphasis is always on enabling individuals to maintain autonomy and engage fully in community life.
Charities and Peer Support Networks
In the UK, charities such as the Spinal Injuries Association (SIA), Back Up Trust, Aspire, and others provide a strong network of support. These organisations offer practical advice, advocacy services, grants for equipment, peer mentoring programmes, and opportunities for social connection. Peer support is especially valued for its unique understanding and encouragement; it often helps reduce feelings of isolation and empowers people to pursue education, employment, or leisure activities.
Holistic Wellbeing and Emotional Health
Long-term wellbeing extends beyond physical health. Psychological resilience is nurtured through access to counselling services, self-help groups, and mindfulness resources. Many NHS trusts now recognise the importance of regular mental health check-ins as part of routine SCI follow-up. Families are also supported to adapt to new roles and challenges through carer networks and respite care options.
Ongoing Advocacy for Quality Improvement
The landscape of long-term SCI management in the UK continues to evolve thanks to advocacy from both professionals and service users. There is a growing focus on inclusive environments, employment opportunities, accessible housing, and digital health innovations that allow for remote monitoring or virtual consultations. Through collaborative efforts between healthcare providers, charities, government agencies, and those living with SCI themselves, best practices are continually refined to ensure lifelong support and dignity.