Introduction to Postural Correction
Postural correction is a cornerstone of physiotherapy practice across the UK, playing a vital role in both preventative care and rehabilitation. The concept refers to the assessment and improvement of an individual’s body alignment, ensuring that the musculoskeletal system functions efficiently during daily activities. In the context of UK physiotherapy, postural correction is not merely about standing up straight; rather, it encompasses a holistic approach that addresses underlying movement patterns, muscular imbalances, and lifestyle factors unique to each patient. Effective postural management can significantly enhance patient well-being, reduce pain, and increase mobility, which are crucial for maintaining independence and quality of life. British physiotherapists often integrate postural education into treatment plans to empower patients with practical strategies they can apply at home, at work, or while engaging in leisure activities. By prioritising optimal posture, physiotherapy professionals help individuals prevent future injuries and manage existing conditions more effectively, fostering long-term health and functional resilience within diverse communities across the UK.
2. Common Postural Issues in the UK Population
Postural problems are a growing concern within the UK, largely due to modern lifestyle habits and work environments. As physiotherapists, it is crucial to understand the specific postural challenges faced by British patients in order to provide effective, patient-centred interventions. The table below outlines some of the most common postural issues observed in the UK population, along with their primary causes and contributing lifestyle factors.
| Postural Issue | Main Causes | Relevant British Lifestyle Factors |
|---|---|---|
| Desk-Based Strains (e.g. forward head posture, rounded shoulders) | Prolonged computer use, poor workstation ergonomics | High prevalence of office-based jobs, widespread remote working culture post-pandemic |
| Lower Back Pain | Sedentary behaviour, inadequate lumbar support, lack of movement breaks | Commuting via car or public transport, long working hours indoors during colder months |
| Tech Neck | Frequent mobile device use, looking down at screens for extended periods | High smartphone adoption, increased use of digital platforms for social connection and work |
| Poor Posture in School-Aged Children | Poorly designed school furniture, heavy backpacks, increased screen time at home and school | Traditional British classroom layouts, emphasis on academic achievement and homework |
| Elderly Kyphosis (excessive upper back curvature) | Age-related muscle weakness, osteoporosis | Aging population with limited access to outdoor activity during winter months |
Lifestyle Habits Unique to the UK:
- Weather Patterns: The UKs often inclement weather discourages outdoor physical activity, contributing to sedentary lifestyles that exacerbate postural issues.
- Cultural Norms: Traditional British etiquette emphasises sitting still and upright for extended periods (e.g. during meetings or social gatherings), often at the expense of natural movement breaks.
- Workplace Trends: Since the COVID-19 pandemic, there has been a significant rise in home-based work. Many individuals lack proper ergonomic setups at home, leading to an increase in musculoskeletal complaints.
- Public Transport Use: Long commutes on buses and trains can encourage slouched or unsupported sitting positions.
By recognising these prevalent postural concerns and the unique contributing factors within British society, physiotherapists can tailor their assessment and intervention strategies more effectively. This patient-centred approach ensures that advice and exercise programmes are not only evidence-based but also relevant to the daily lives of those living in the UK.
3. Assessment Techniques Used by UK Physiotherapists
Accurate assessment is the cornerstone of effective postural correction in UK physiotherapy practice. Chartered physiotherapists employ a range of evidence-based assessment methods to identify postural imbalances and tailor interventions to individual needs. Central to this approach is adherence to the latest guidelines from professional bodies such as the Chartered Society of Physiotherapy (CSP) and the National Institute for Health and Care Excellence (NICE).
Comprehensive Subjective Assessment
The assessment process begins with a thorough subjective evaluation, where physiotherapists explore the patient’s history, daily activities, occupational demands, and any presenting symptoms. This stage is crucial for understanding potential contributing factors to postural issues, including lifestyle, repetitive movements, or previous injuries.
Objective Postural Analysis
Physiotherapists in the UK commonly use visual observation and validated screening tools to analyse static and dynamic posture. Tools such as the Modified Oswestry Disability Index or the Visual Analogue Scale may be utilised to quantify functional impairment. During observation, attention is given to alignment of major joints, spinal curves, weight distribution, and asymmetries that may indicate muscular imbalances or compensatory patterns.
Functional Movement Screening
Functional assessments—including squat tests, gait analysis, and balance tests—allow clinicians to evaluate how postural deviations impact movement quality. These assessments help in identifying weaknesses or restrictions that may not be apparent during static examination alone.
Special Tests and Manual Palpation
Manual palpation and specific clinical tests, such as spinal mobility assessments or muscle length tests (e.g., Thomas test for hip flexors), are frequently incorporated. These hands-on techniques provide valuable insight into soft tissue tension, joint range of motion, and neuromuscular control relevant to posture.
Clinical Reasoning and Individualised Approach
UK physiotherapists integrate findings from both subjective and objective assessments using advanced clinical reasoning skills. By synthesising information from multiple sources, clinicians ensure their diagnosis aligns with current best evidence while respecting each patient’s unique context and goals. This person-centred approach not only guides targeted intervention but also enhances patient engagement throughout their rehabilitation journey.
4. Core Principles of Postural Correction
Postural correction within UK physiotherapy is grounded in a set of core principles that ensure interventions are both evidence-based and tailored to the individual needs of each patient. Understanding these principles is essential for effective management and long-term success in addressing postural dysfunction.
Movement Analysis
Comprehensive movement analysis forms the foundation of any postural correction strategy. Physiotherapists in the UK utilise detailed assessments to observe how patients perform everyday activities, such as walking, sitting, or lifting. This process helps to identify abnormal movement patterns, compensations, and areas of potential risk. Accurate movement analysis not only guides targeted interventions but also allows for measurable progress over time.
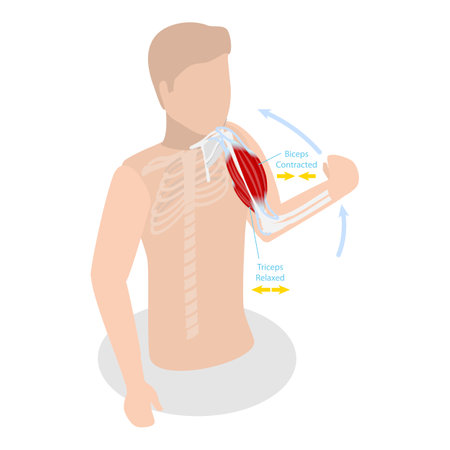
Muscle Balance
Achieving optimal muscle balance is a key objective in postural correction. Imbalances often result from overuse, underuse, or injury, leading to altered posture and function. Physiotherapists employ specific techniques to restore equilibrium between agonist and antagonist muscle groups. The following table summarises common examples:
| Muscle Group | Common Imbalance | Correction Strategy |
|---|---|---|
| Upper back vs Chest | Tight pectorals & weak rhomboids/trapezius | Stretch chest muscles, strengthen upper back |
| Abdominals vs Lower back | Weak abdominals & tight lumbar extensors | Core strengthening & lumbar stretching |
| Hip flexors vs Gluteals | Tight hip flexors & weak gluteals | Lengthen hip flexors, activate gluteal muscles |
Patient-Centred Goal Setting
A hallmark of UK physiotherapy practice is its commitment to patient-centred care. Collaborative goal setting ensures that treatment aligns with each patients lifestyle, functional demands, and personal aspirations. By involving patients in decision-making and prioritising their individual goals—whether returning to work, resuming sport, or simply reducing daily discomfort—physiotherapists foster greater motivation and adherence to rehabilitation plans.
Summary of Fundamental Principles
| Principle | Description in Practice (UK) |
|---|---|
| Movement Analysis | Detailed observation and assessment during functional tasks; ongoing reassessment to track progress. |
| Muscle Balance Restoration | Targeted exercises and manual therapy aimed at correcting identified imbalances. |
| Patient-Centred Goals | Shared decision-making with achievable milestones tailored to the individuals needs. |
Together, these core principles underpin all aspects of postural correction in the UK, ensuring interventions are holistic, effective, and sustainable for every patient.
5. Patient Education and Engagement
Within UK physiotherapy practice, patient education and engagement form the cornerstone of effective postural correction. British physiotherapists recognise that lasting improvements are best achieved when patients are empowered to take an active role in their own care. This is accomplished through a multifaceted approach involving personalised advice, lifestyle modification, and self-management strategies tailored to the unique needs and circumstances of each individual.
Personalised Advice for Every Patient
UK physiotherapists pride themselves on delivering advice that is not only evidence-based but also deeply relevant to each patients lifestyle and daily activities. During consultations, practitioners assess work environments, home setups, and leisure pursuits—whether it’s sitting at a desk in a London office or gardening in the countryside—to provide practical guidance that resonates with local routines. This bespoke approach ensures that recommendations are realistic and easily integrated into everyday life.
Lifestyle Modification: Supporting Change
Understanding that poor posture often stems from habitual patterns, British physiotherapists guide patients through meaningful lifestyle changes. This might involve ergonomic adjustments at workstations compliant with UK health and safety standards, encouragement to utilise public transport options more actively, or recommendations for community-based physical activities such as walking groups or local sports clubs. These suggestions not only address posture but also support broader wellbeing within the context of the UK’s diverse living environments.
Promoting Self-Management Strategies
A key aspect of UK physiotherapy is equipping patients with the skills to monitor and improve their posture independently. Practitioners introduce simple self-assessment techniques, smartphone apps popular within the UK, and home exercise routines that empower individuals to manage symptoms between appointments. Educational materials are provided in plain English, often reflecting NHS guidelines, ensuring accessibility for all backgrounds.
Building Long-Term Engagement
The ongoing relationship between patient and physiotherapist is highly valued in the UK. Regular follow-up sessions—either face-to-face or via digital platforms—allow for progress reviews and further adaptation of strategies as needed. By fostering open communication, trust, and collaboration, UK physiotherapists create an environment where patients feel supported throughout their journey towards optimal postural health.
6. Integration of Postural Correction into Everyday Life
Practical Strategies for Work Environments
For many individuals in the UK, a significant portion of the day is spent at work—often at a desk or workstation. Encouraging patients to adopt correct postural habits starts with small but consistent changes. Remind patients to adjust their chair height so feet are flat on the floor, keep their screen at eye level, and support their lower back with a cushion if needed. Suggest setting reminders every hour to stand up, stretch, or walk around the office. For those working from home, recommend investing in ergonomic equipment or improvising with household items to create a supportive workspace. Encourage participation in workplace wellbeing initiatives, such as lunchtime walking clubs or standing meetings, which are increasingly popular across British workplaces.
Applying Postural Principles at Home
At home, daily routines present ample opportunities for reinforcing postural correction. Advise patients to be mindful of posture during common activities like cooking, gardening, or even relaxing on the sofa. Recommend switching sitting positions regularly and using cushions for lumbar support while watching television. For parents and carers, highlight the importance of safe lifting techniques when handling children or household objects—bend the knees and keep the back straight to reduce strain. Encourage family involvement by making postural exercises a group activity, turning it into an enjoyable part of evening routines.
Leisure Activities and Social Engagement
British social culture often involves pub gatherings, sporting events, or leisurely walks in local parks. Guide patients to apply postural awareness during these occasions—for example, maintaining upright posture while standing at social events or taking regular breaks when seated for extended periods. Suggest incorporating gentle exercises like Pilates, yoga, or swimming—activities widely available through community centres and leisure clubs across the UK—to strengthen postural muscles. Emphasise that improvements can be seamlessly integrated into hobbies such as cycling along scenic routes or participating in village cricket matches.
Building Sustainable Habits
Ultimately, the goal is to help patients make postural correction a natural part of their lifestyle rather than an added burden. Encourage setting realistic goals and celebrating small successes along the way. Provide resources such as NHS-approved apps or local support groups where individuals can share progress and tips. By fostering self-awareness and gradually embedding positive habits into daily routines, patients are more likely to achieve long-term benefits and enjoy an active, pain-free life within the vibrant context of British living.
7. Multi-Disciplinary Collaboration in UK Healthcare
Effective postural correction in UK physiotherapy practice is seldom achieved in isolation. Collaboration with a range of healthcare professionals and services, both within the NHS and private sectors, is fundamental to providing holistic and patient-centred care. Physiotherapists regularly work alongside GPs, occupational therapists, orthopaedic consultants, podiatrists, and even mental health professionals to ensure that all factors contributing to postural issues are addressed. This team-based approach allows for comprehensive assessment and management, drawing on the unique expertise of each discipline to create tailored rehabilitation programmes.
Within the NHS framework, multi-disciplinary team (MDT) meetings are a cornerstone of integrated care. These meetings facilitate open communication and shared decision-making between professionals, ensuring that the patient’s physical, psychological, and social needs are considered in their postural correction plan. In private practice settings, physiotherapists often establish strong referral networks with local clinicians and specialists, enabling timely access to diagnostics or adjunct therapies such as sports massage, pilates instruction, or ergonomic assessments.
The benefit of this collaborative approach extends beyond clinical outcomes; it also enhances patient engagement and satisfaction by providing clear information, coordinated appointments, and seamless transitions between services. By prioritising multi-disciplinary collaboration, UK physiotherapists uphold the highest standards of practice—delivering holistic solutions that support sustainable postural health for patients across diverse settings.


