Introduction to Fascia
Fascia, once considered merely a passive connective tissue, has recently emerged as a subject of considerable fascination among manual therapists and healthcare professionals across the UK. This delicate yet robust network of fibrous tissue weaves throughout the entire body, enveloping muscles, organs, nerves, and blood vessels in an intricate web. Far from being an inert wrapping, fascia plays a pivotal role in structural support, movement coordination, and even communication within our bodies. Its remarkable adaptability and responsiveness to physical demands have prompted renewed interest, especially as more evidence highlights its influence on mobility, pain management, and overall well-being. In recent years, British practitioners have increasingly embraced fascia-focused therapies, seeking gentle yet effective approaches to soft tissue mobilisation that are both rooted in science and tailored to individual needs. As we begin this exploration into fascia, it is important to understand not only its structure but also why this connective tissue is now at the forefront of evidence-based practice in the realm of manual therapy.
2. Current Evidence on Fascia Function and Dysfunction
Recent years have seen a surge of interest in fascia within both UK-based and international research communities, bringing greater understanding to this often-overlooked tissue. Fascia, a connective tissue network, plays a vital role in supporting movement, contributing to pain syndromes, and responding to injury. This section draws upon reputable sources such as the British Journal of Sports Medicine, NHS guidelines, and leading global studies to clarify the functional and dysfunctional aspects of fascia.
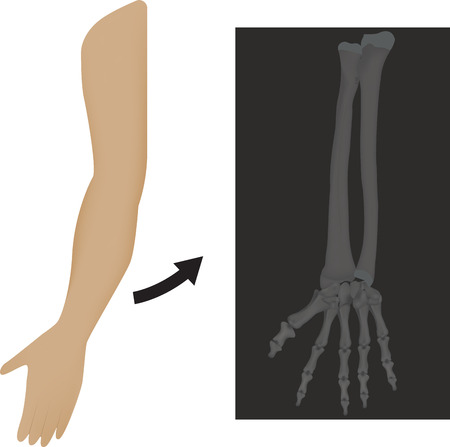
The Role of Fascia in Movement
Fascia provides a continuous sheath that envelops muscles, bones, nerves, and organs. UK researchers from institutions like University College London (UCL) have highlighted its role in transmitting force and allowing smooth gliding between muscle groups. When healthy, fascia maintains flexibility and resilience, supporting efficient and coordinated movement essential for daily living—an important consideration for individuals receiving long-term care or those aiming to remain independent.
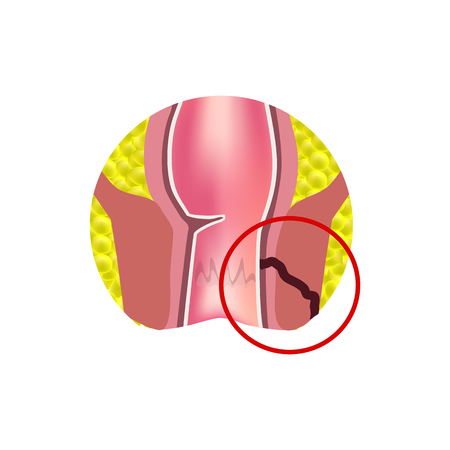
Fascia’s Contribution to Pain
A growing body of evidence indicates that fascial dysfunction can contribute significantly to chronic pain conditions. The NHS recognises myofascial pain syndrome as a common concern, especially among older adults or those with limited mobility. International studies suggest that restricted fascia may result in localised pain or referred discomfort due to nerve entrapment or altered biomechanics.
| Aspect | Normal Fascia Function | Dysfunctional Fascia |
|---|---|---|
| Movement | Smooth gliding, force transmission | Stiffness, reduced range of motion |
| Pain Response | Minimal discomfort with activity | Chronic ache, sensitivity or referred pain |
| Response to Injury | Promotes repair via cell signalling | Scar tissue formation, persistent inflammation |
Responses to Injury: Insights from Research
Both UK and international studies reveal that after injury or surgery, fascia may become thickened or less elastic—a process associated with scarring (fibrosis). For example, research published by Kings College London demonstrates that targeted mobilisation techniques can help reduce fascial adhesions post-injury, improving function for patients recovering from hip fractures or joint replacements. This evidence underpins many soft tissue mobilisation interventions now recommended across NHS physiotherapy services.
A Gentle Reminder for Practice
Understanding the latest scientific perspectives on fascia helps therapists and carers select more effective mobilisation approaches tailored to each individual’s needs. Whether you are supporting someone at home or working within the healthcare system, staying updated with current evidence ensures compassionate care that respects both comfort and dignity.
3. Principles of Soft Tissue Mobilisation
When considering soft tissue mobilisation within the context of fascia, it is important to emphasise evidence-based techniques that have gained widespread acceptance across Britain. These approaches are grounded in research and clinical experience, ensuring both safety and effectiveness for individuals seeking relief from discomfort or improved mobility.
Myofascial Release
Myofascial release remains one of the most frequently used methods for addressing fascial restrictions. This technique involves gentle, sustained pressure on areas of tension within the fascia, allowing for gradual elongation and increased pliability of connective tissues. Practitioners in the UK are trained to perform myofascial release with a focus on patient comfort, applying just enough pressure to facilitate change without causing pain or undue stress.
Gentle Manual Therapy
Another core principle in British practice is the use of gentle manual therapy. Techniques such as soft tissue massage, trigger point therapy, and light stretching are applied with sensitivity to the individual’s needs and overall health status. The aim is always to support natural healing processes rather than forcing change, which aligns with person-centred care values cherished in British healthcare.
Safety and Effectiveness
Evidence-based practice prioritises safety above all else. Practitioners assess each person thoroughly before commencing treatment, taking into account medical history, current symptoms, and any contraindications. This careful approach ensures interventions remain suitable for those living with chronic conditions or age-related concerns—a reflection of long-term care principles integral to UK practice.
Collaboration and Communication
A crucial aspect underpinning these techniques is open communication between practitioner and client. By explaining each step and encouraging feedback, therapists foster trust and reassurance—vital elements for anyone who may feel apprehensive about physical therapies. This collaborative style not only improves outcomes but also exemplifies the gentle companionship valued throughout British long-term care settings.
Through a combination of myofascial release, gentle manual therapy, and a steadfast commitment to safety, practitioners in Britain offer soft tissue mobilisation that respects both scientific evidence and the unique needs of every individual.
4. Clinical Applications and Patient-Centred Care
In the context of both the NHS and private practice in the UK, fascia-focused soft tissue mobilisation is becoming increasingly recognised as a valuable element of holistic care. Successfully integrating evidence-based approaches to fascia into clinical settings requires sensitivity to individual patient needs, preferences, and expectations. By tailoring interventions and communication, practitioners can foster trust and achieve better therapeutic outcomes.
Integrating Fascia-Focused Care: Practical Tips
To bridge scientific understanding and everyday clinical application, consider these practical strategies for providing fascia-informed care:
| Clinical Setting | Practical Tip | Patient Benefit |
|---|---|---|
| NHS Outpatient Clinic | Begin with a thorough assessment including patient history and movement analysis; explain fascia’s role in simple terms. | Improved engagement and understanding of treatment rationale. |
| Private Practice | Offer flexible appointment lengths for more comprehensive hands-on techniques and guided self-care education. | Bespoke interventions supporting autonomy and well-being. |
| Multidisciplinary Team Settings | Liaise with physiotherapists, occupational therapists, or GPs about shared fascia-related findings and progress. | Consistent messaging and collaborative care pathway. |
| Community/Home Visits | Adapt manual techniques for comfort; provide simple tools (e.g., foam rollers) for home use where appropriate. | Sustained self-management outside of clinic hours. |
Adapting to Individual Needs and Preferences
The success of fascia-focused approaches lies not only in technical skill but also in the practitioner’s ability to listen actively and respond empathetically. Consider factors such as pain tolerance, cultural attitudes towards touch, age-related changes in tissue elasticity, and previous experiences with manual therapy. For example:
- Elderly patients: Use gentler pressure and slower techniques; reassure regarding safety and expected sensations.
- Younger adults: Incorporate education around posture, activity modification, and self-release methods for long-term benefit.
- Cultural diversity: Seek consent at every stage, respect boundaries around physical contact, and use language that honours individual perspectives on health.
The Role of Communication in Patient-Centred Fascia Care
Cultivating open dialogue helps demystify soft tissue mobilisation. Encourage questions, clarify goals collaboratively, and regularly review progress together. This patient-centred approach aligns closely with NHS values of dignity, respect, and partnership—ensuring that each intervention is meaningful to those receiving it.
5. Considerations and Contraindications
While soft tissue mobilisation and fascia-focused techniques offer promising benefits, it is essential to recognise that these approaches are not universally suitable. Careful assessment forms the cornerstone of safe practice, particularly within the context of long-term care where individuals may present with complex health needs or vulnerabilities. Before initiating any intervention, it is crucial to identify potential contraindications such as active infection, open wounds, recent surgery, severe osteoporosis, or unexplained pain. In addition, conditions like deep vein thrombosis or certain skin disorders may render fascia techniques inappropriate.
Safeguarding and Assessment
Professional judgement should guide every decision, with safeguarding firmly at the forefront. Comprehensive assessment involves reviewing medical history, understanding current medications, and liaising with multidisciplinary teams where necessary. This collaborative approach ensures that interventions respect both physical safety and emotional well-being, especially for those living with dementia or reduced communication abilities.
Promoting Dignity in Practice
Dignity and respect must underpin all interactions in long-term care settings. Practitioners should always seek informed consent, explaining procedures in clear, reassuring language tailored to each individual’s level of understanding. Maintaining privacy—by ensuring appropriate draping and a calm environment—also helps foster trust and comfort throughout the process.
Adapting Approaches for Individual Needs
No two people are alike; thus, techniques should be adapted to suit unique preferences and health profiles. If there are any doubts regarding suitability or if an individual expresses discomfort at any stage, it is best to pause and review the approach. Ultimately, prioritising safety, dignity, and person-centred care ensures that evidence-based fascia mobilisation remains a supportive—not harmful—component of holistic wellbeing.
6. Future Directions and Continuing Education
As our understanding of fascia continues to evolve, so too does the landscape of soft tissue mobilisation practice in the UK. The latest research is shining a light on the intricate ways fascia communicates with muscles, nerves, and even our immune system, suggesting that gentle, evidence-based approaches may offer more than just physical benefits—they can support overall wellbeing.
Emerging Trends in Fascia Research
Recent studies highlight the dynamic nature of fascia, focusing on its adaptability and responsiveness to movement and manual therapy. Advanced imaging techniques are allowing researchers to observe fascia in action, which is helping therapists tailor interventions for conditions ranging from chronic pain to sports injuries. Keeping abreast of these developments enables UK practitioners to provide care rooted in the most up-to-date scientific evidence.
The Importance of Ongoing Training
For therapists across the UK, ongoing professional development is not just a regulatory requirement—it’s a way to ensure clients receive safe, effective care. Workshops, online courses, and peer-reviewed journals offer opportunities to deepen knowledge about fascia and refine soft tissue mobilisation skills. Engaging with local professional bodies such as the Chartered Society of Physiotherapy or the British Fascia Symposium can foster supportive learning communities.
Gentle Learning Resources
If you wish to continue your journey into fascia-informed practice, consider seeking out resources that emphasise kindness—to both practitioner and client. Gentle learning might include attending webinars focused on trauma-sensitive touch or reading books that combine clinical expertise with compassionate perspectives. Podcasts and discussion groups dedicated to soft tissue therapy can also provide encouragement and fresh insights in a friendly, accessible format.
As we look forward, embracing emerging research alongside continuous education ensures that fascia-focused care in the UK remains both progressive and deeply nurturing—for therapists and those they support alike.