Understanding Community-Based Rehabilitation Services
Community-based rehabilitation (CBR) services are designed to support individuals with disabilities or long-term health conditions within their own communities. The core purpose of CBR is to promote social inclusion, independence, and quality of life by providing accessible and locally tailored rehabilitation options. These services work in partnership with the NHS and local authorities, ensuring that people receive comprehensive care close to home. CBR encompasses a wide range of support, including physiotherapy, occupational therapy, speech and language therapy, as well as social and psychological assistance. By focusing on the unique needs of each community, these services aim to empower individuals to manage their health conditions, participate fully in everyday life, and remain connected with their families and social networks.
2. Eligibility and Referral Pathways in the NHS
Community-Based Rehabilitation (CBR) services play a crucial role in supporting individuals to regain independence and improve their quality of life following illness, injury, or disability. Accessing these services through the NHS involves understanding both who is eligible and how referrals are managed within the system.
Who Can Access CBR Services?
CBR services are designed for people of all ages who require rehabilitation to enhance their physical, psychological, or social wellbeing. This includes:
- Adults recovering from stroke, surgery, or major illness
- Individuals with long-term conditions such as Parkinson’s disease or multiple sclerosis
- Children with developmental delays or disabilities
- Elderly patients aiming to maintain independence at home
Eligibility Criteria
The NHS applies specific eligibility criteria to ensure those most in need receive support. While criteria may vary between localities, typical factors considered include:
| Eligibility Factor | Description |
|---|---|
| Clinical Need | Assessment by a healthcare professional to determine rehabilitation requirements |
| Level of Function | Impact of condition on daily living activities and independence |
| Medical Stability | Individual must be medically stable and able to engage in rehabilitation safely |
| Potential for Improvement | Likelihood that rehabilitation will lead to meaningful gains in function or quality of life |
NHS Referral Pathways Explained
The NHS operates a structured referral process for accessing CBR services. Generally, individuals cannot self-refer; instead, a healthcare professional—such as a GP, hospital consultant, or community nurse—assesses the individual’s needs and initiates a referral if appropriate. The steps usually include:
- Initial Assessment: Conducted by a healthcare provider to identify needs and suitability for CBR.
- Referral Submission: A formal referral is made to the relevant NHS rehabilitation team or service provider.
- Multidisciplinary Review: A team of professionals reviews the referral and determines the most suitable intervention plan.
- Service Allocation: If eligible, the individual is matched with appropriate community-based rehabilitation support tailored to their goals.
Key Points for Patients and Carers
- If you believe you or someone you care for would benefit from CBR, speak to your GP or primary healthcare professional for advice on next steps.
- NHS services aim to provide equitable access across England, Scotland, Wales, and Northern Ireland; however, local variations in service provision may exist.
- Your care team will keep you informed throughout the process and involve you in decisions about your rehabilitation pathway.
This patient-centred approach ensures that each individual receives timely support tailored to their unique needs within the UK’s healthcare framework.
3. The Patient Journey: What to Expect
Navigating community-based rehabilitation services through the NHS is a structured process designed around the needs and preferences of each individual. Understanding what to expect at each stage can help patients and their families feel more confident and supported throughout their rehabilitation journey.
Initial Assessment
The journey typically begins with an initial assessment, which may be arranged by your GP, hospital team, or another healthcare professional. During this stage, a multidisciplinary team—often including physiotherapists, occupational therapists, and other specialists—will evaluate your condition, discuss your goals, and identify the most appropriate support for your needs. This assessment is patient-centred, meaning you are encouraged to share your own priorities and concerns so that the care plan reflects what matters most to you.
Developing Your Care Plan
Following the assessment, you and your healthcare team will work together to develop a personalised care plan. This plan outlines the recommended therapies, frequency of sessions, and any equipment or support services required. Key points of contact, such as your main therapist or case coordinator, will be introduced to ensure you always know whom to approach with questions or concerns.
Accessing Ongoing Support
Once your care plan is in place, regular sessions or visits will begin either in your home or at a local community facility. Throughout this period, the focus remains on empowering you to achieve greater independence and improve your quality of life. Progress is reviewed regularly, with adjustments made as needed based on your feedback and evolving needs.
Patient-Centred Approach
The NHS is committed to placing patients at the heart of every decision. You will be actively involved in setting goals and monitoring outcomes, ensuring that support remains relevant and effective. Family members or carers are also welcome to participate in discussions if you wish.
Key Points of Contact
Throughout your rehabilitation journey, clear communication channels are maintained. You will have designated points of contact within your care team—such as a lead therapist or rehabilitation coordinator—who can provide guidance, answer queries, and help navigate any challenges that arise along the way.
4. Multidisciplinary Teams and Collaborative Care
Community-Based Rehabilitation (CBR) services accessed through the NHS are delivered by a network of health and social care professionals who work together to provide holistic support tailored to each individual’s needs. This collaborative approach ensures that patients benefit from a wide range of expertise, leading to more effective and personalised rehabilitation outcomes.
The Roles of Health and Social Care Professionals
CBR is underpinned by multidisciplinary teams (MDTs), which bring together specialists from various fields. These professionals collaborate closely, sharing their knowledge and skills to develop comprehensive care plans for patients. The table below outlines the key roles typically involved in delivering CBR through the NHS:
| Professional Role | Main Responsibilities |
|---|---|
| Physiotherapist | Assesses and develops programmes to improve mobility, strength, and physical function. |
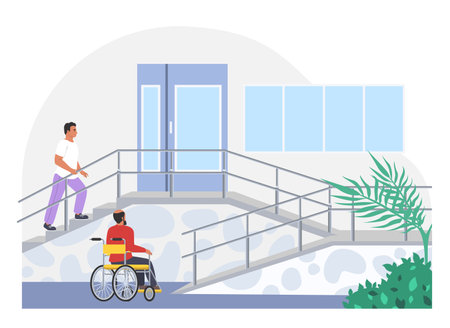
| Occupational Therapist | Supports individuals with daily living activities and recommends adaptations or equipment. |
| Speech and Language Therapist | Helps with communication or swallowing difficulties resulting from injury or illness. |
| Nurse | Provides ongoing medical care, monitors health conditions, and supports medication management. |
| Social Worker | Assists with access to community resources, benefits, and emotional support for patients and families. |
| Psychologist or Counsellor | Addresses mental health challenges, offering therapeutic interventions as required. |
| Rehabilitation Support Worker | Aids therapists in implementing care plans and supporting patients’ independence at home. |
The Importance of Collaboration in Patient Wellbeing
Effective communication and regular meetings among MDT members are essential for coordinated care. By working collaboratively, professionals ensure that each aspect of a patient’s wellbeing is considered—whether it be physical, emotional, or social. This not only enhances recovery but also empowers patients to achieve their personal goals within their community setting.
5. Accessing Support and Overcoming Barriers
Accessing community-based rehabilitation (CBR) services through the NHS can sometimes feel daunting, but there are practical steps and resources to support you every step of the way. Understanding your options and knowing where to find help can make a significant difference in your rehabilitation journey.
How to Seek Help
The first step is to speak with your GP or healthcare professional, who can assess your needs and refer you to appropriate CBR services. It’s helpful to be open about your challenges and goals, so they can tailor their recommendations. If you already have a care plan in place, ask for it to be reviewed if your circumstances change or if you feel your current support is not meeting your needs.
Resources Available
NHS Rehabilitation Services
The NHS provides a range of CBR services, including physiotherapy, occupational therapy, speech and language therapy, and mental health support. These may be offered at local health centres, in your home, or through outreach programmes. Your local Clinical Commissioning Group (CCG) or Integrated Care Board (ICB) can provide information on what is available in your area.
Community Organisations
Charities such as Scope, Age UK, and Mind offer additional advice and support for those navigating rehabilitation services. Many also run peer support groups and activities that help reduce isolation and promote wellbeing.
Overcoming Common Challenges
Dealing with Waiting Times
If you encounter long waiting lists, ask your GP about interim self-management strategies or alternative local services while you wait. Some therapies may also be available digitally or via telephone consultations.
Understanding Your Rights
You have the right to be involved in decisions about your care. If you feel your voice isn’t being heard, consider bringing a family member or advocate to appointments. You can also request written information or ask for a second opinion if needed.
Top Tips for Success
- Keep a record of symptoms and progress to share during appointments.
- Don’t hesitate to follow up on referrals if you haven’t heard back within expected timeframes.
- Reach out to local patient advice and liaison services (PALS) for guidance if you face difficulties accessing care.
- Engage with community groups for additional emotional and practical support.
Remember, seeking help is a sign of strength, not weakness. By making use of available resources and advocating for yourself, you can overcome barriers and access the rehabilitation support you deserve through the NHS.
Community Resources and Support Networks
Beyond the services offered directly by the NHS, there is a wealth of community resources and support networks across the UK that can significantly enhance your rehabilitation journey. Many local groups and charities work closely with NHS teams to provide practical assistance, emotional support, and opportunities for social engagement that help promote lasting community integration.
Charities such as Age UK, Scope, Mind, and the Stroke Association offer tailored programmes and peer support groups that cater to specific conditions or age groups. These organisations often run local activities—from exercise classes and workshops to befriending schemes—that complement NHS rehabilitation plans, helping you stay active and connected in your community.
Your local council website or GP surgery is an excellent starting point for finding out what’s available in your area. Many regions have Community Rehabilitation Teams who maintain up-to-date directories of voluntary sector services, carers’ groups, transport schemes, and accessible leisure facilities. Engaging with these resources can help bridge any gaps between formal healthcare and everyday living, making it easier to adapt after illness or injury.
Support networks extend beyond medical needs; many community centres and faith-based organisations provide drop-in sessions where you can meet others facing similar challenges. These informal settings foster shared understanding, encourage independence, and reduce feelings of isolation during recovery.
Finally, don’t hesitate to ask your NHS rehabilitation team about signposting to trusted local resources or how to self-refer to relevant organisations. By tapping into these wider networks, you’ll benefit from a more holistic approach that supports not only your physical recovery but also your overall wellbeing as you reintegrate into everyday life.


